Climate Change: Could it give rise to the next viral disease outbreak?

The effects of global warming can strike with little warning or build up gradually over time. Providers cannot afford to wait to prepare for its potential impacts.
Ask health futurist and medical economist Jeffrey Bauer, PhD, what he thinks will be among the most consequential changes affecting healthcare the next five to 10 years, and you can be sure climate change will be at the top of the list.a
That answer is not surprising given that his first career choice was research meteorology and climate science. In the 1960s, Bauer was working for the National Center for Atmospheric Research in Boulder, Colorado, when his draft board sent him to alternative service at a 300-bed hospital. After two years of direct involvement in clinical care, the hospital leader, a Catholic nun, convinced him to pursue a PhD in medical economics, and he would go on to become a recognized authority and author of more than 300 books, articles, videos and web pages on the U.S. healthcare system.
Climate change may not seem like an obvious first choice, because at any given time and place, its effects tend to be hidden under a veil of normalcy. Yet Bauer agrees with the 97% of all published climate scientists who see climate change as an urgent reality driven by human activity.b He also suggested healthcare providers are only beginning to understand this reality.
“More frequent and intense hurricanes and tornadoes, fires, drought, extreme heat and cold, and rising sea levels will all create major problems for providers much sooner than expected,” he said. “And depression, trauma, infectious diseases and other environmentally linked diseases will create many new demands for which healthcare is poorly prepared.”
Bauer said the challenge for healthcare is compounded by relative inaction at the federal level, resulting from the controversial U.S. withdrawal from the Paris Climate Agreement, the lack of legislation to address climate change due to partisan discord in Congress and the president’s rejection of the scientific community’s consensus on climate change.c
“Given the political system’s inability to prepare for climate change, I’m not sure that health professionals and provider organizations can do much of anything other than responding on an ad hoc basis in the context of the local climate and economy,” Bauer said.
The nature of the threat
Bauer cited many examples, both obvious and subtle, of climate change’s effects on healthcare.
The spread of infectious disease. Vector-borne illnesses, particularly those spread by mosquitoes, are expanding into regions of the United States where they have not been seen before.d “With a change in the average temperature in a climate by one degree, the types of mosquitoes that carry those viruses move hundreds and hundreds of miles north.” As a result, there is an increased possibility hospitals in many southern states, and even in states like Illinois, Indiana and Kentucky, may encounter mosquito-borne viruses they are not accustomed to seeing, including West Nile disease, Dengue fever and Zika virus disease.e The current crisis with COVID-19, although not specifically linked to climate change, is a sobering reminder of how great a threat infectious diseases can pose, including those that can extend their reach as a result of global warming.
Extreme temperatures. Hotter summers increase the incidence of depression and exacerbate chronic health conditions. “People with congestive heart failure tend to have much higher death rates in a hot summer. What if every summer is getting hotter?”
For a CFO, increased temperature extremes also are a concern because they translate into higher operating costs from the need for additional air conditioning or heating: “Hospitals in the north are seeing new lows and new highs,” he said. “In a way, it’s a misnomer to talk only about ‘global warming’ because the same places experiencing warming summers are also having colder winters. And that has an enormous impact on a hospital’s utility bills. The hospitals may need to install more thermally efficient windows because the additional heating and air conditioning costs can far exceed the costs of the improvements.”
More intense storms. Bauer also cited the high-profile impacts of climate change from superstorms like Hurricane Katrina and Hurricane Sandy, and from floods in the South and Midwest. Many hospitals require substantial reengineering to withstand such storms and to avoid having to transport patients because of lost power, he said.
Droughts from shifting patterns of precipitation. Climate change can have unseen impacts in the local economy across the country, especially in agricultural areas, Bauer said. “Agriculture is no longer capable of supporting a good deal of rural America. And as you lose agriculture due to the climate, then you lose some local economic base as more people move away from those rural areas to find better economic opportunities elsewhere. I read a story recently about high schools in rural Illinois that had to go from 11-man to six-man football teams because the population had dwindled so much they didn’t have enough players to field a whole team.” Bauer concluded that a drought-driven economic decline leading to that kind of population loss would have far greater consequences for healthcare.
A hypothetical impact of climate change on a population’s access to healthcare
Climate change has the potential to produce many unanticipated effects on healthcare access and payment, according to Bauer. He offered California as an example, noting the state has been able to generate an amazingly progressive education and healthcare system largely because of its broad and relatively wealthy population base.
“I think there’s a general consensus around the country that MediCal is the most generous Medicaid program in the country,” he said. “And that’s going to fall apart If suddenly California starts dealing with declining budgets due to declining populations, which it had never seen before.”
Climate change is a key factor that could lead to such a population decline. Bauer suggested it’s possible people could eventually decide they don’t want to live in a place that has constant droughts and fires, with incessant widespread smoke damage and the threat of mudslides from burned slopes that could collapse in monsoon rains. Any serious population decline would lead to a loss in tax revenue that could reduce the California government’s capacity to deliver the same level of public services, potentially resulting in a far less robust Medicaid program.
What comes next
The trajectory of the response to climate change in the U.S. appears promising, despite the relative inaction by the federal government, suggested David Blumenthal, MD, president of The Commonwealth Fund. Blumenthal is an outspoken advocate for action on climate change, who also believes there is an awakening going on across the nation about the issue.e
“Paradoxically the backing away by our federal government from this topic has focused the private sector much more on it,” Blumenthal said. “And healthcare is probably in that group.”
Blumenthal has observed, and written about, the U.S. healthcare system being a massive source of carbon dioxide emissions in the atmosphere. He observed that the gross domestic product of the U.S. healthcare system is 18% of the largest gross domestic product in the world, which is comparable in size to the financial activity of many moderate to middle-sized countries.g
“In any U.S. national goals around containing carbon emissions, the healthcare system would have to be a major part of that activity,” Blumenthal said. “And that means a new emphasis on carbon neutrality, breeding of facilities, increased efficiency of heating and lighting, reduced waste, and more careful thinking about the use of disposables and how to reuse things safely.
“There’s a leadership opportunity here,” Blumenthal continued. “As the public becomes more attuned to climate change as an issue, as I think they are, then being the hospital in your community that has a big banner outside saying ‘we’re carbon neutral’ or ‘we’re Green’ could be a public relations advantage. And once one organization does that, everyone else is going to have to catch up.”
7 steps to protect providers from the perils of climate change
Hospitals and health system leaders need to consider all the dangers of global warming that could threaten their organizations as they prepare for the impending risks.

Georges C. Benjamin, MD, executive director of the American Public Health Association, has been a vocal advocate for action on climate change, having presented witness testimony on the topic before The House Committee on the Budget on July 24, 2019.h Benjamin recommended that healthcare organizations take the following steps to ensure their organizations are fully prepared for the impact of climate change.
1. Perform a risk assessment. “Hospitals and health systems need to sit down and really take stock of the specific threats affecting their particular areas and come up with a plan to prepare for those threats,” Benjamin said.
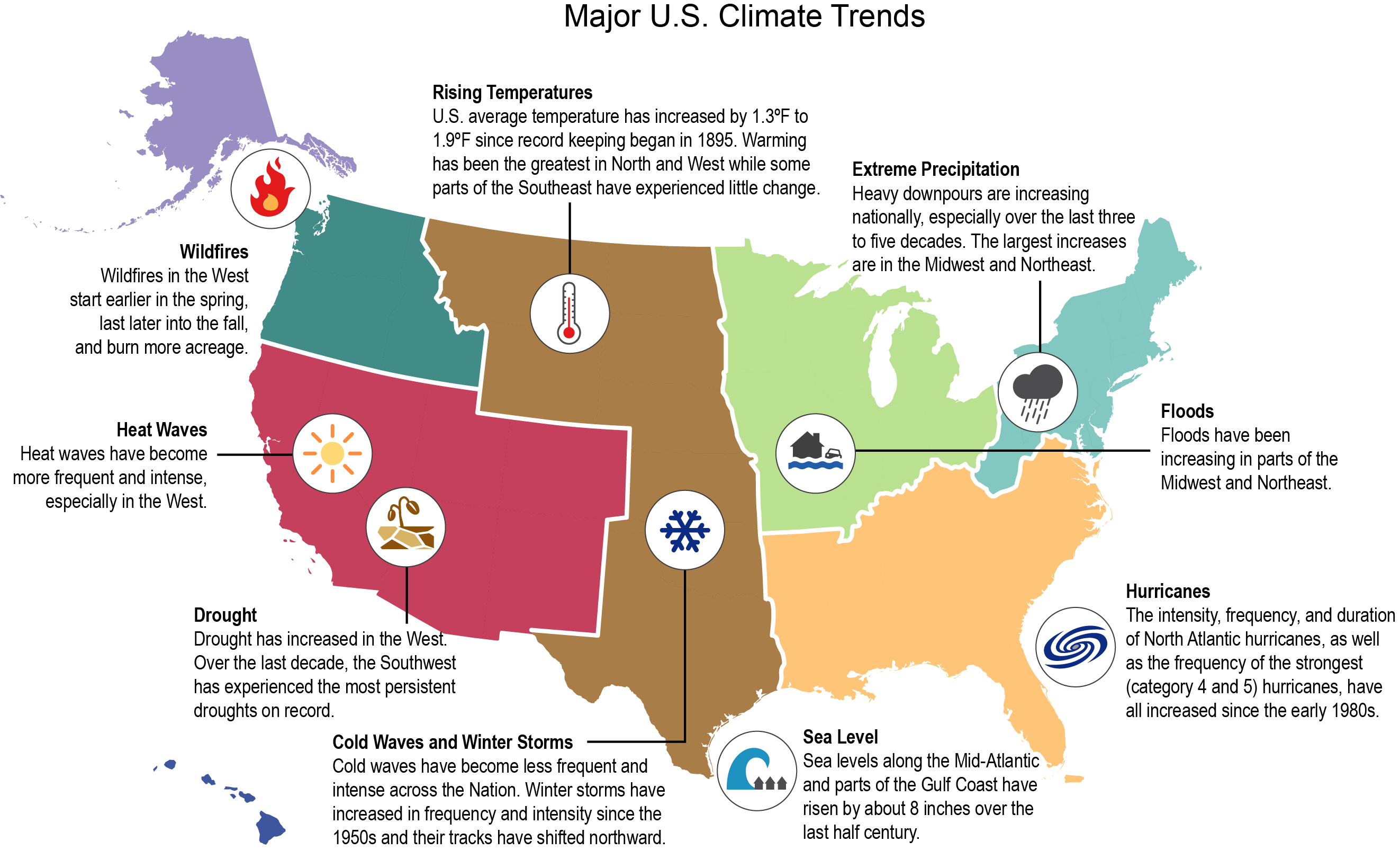
Source: Adapted from Balbus, J., Crimmins, A., Gamble, J.L., Easterling, D.R., Kunkel, K.E., Saha, S. and Sarofim, M.C., “Ch. 1: Introduction: Climate Change and Human Health,” The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment, 2016, U.S. Global Change Research Program, Washington, D.C., Used with permission.
2. Take steps to mitigate the possible adverse impact on billing and collections. Benjamin recommended maintaining duplicate patient records billing systems in a place separate from the facility. “Because if the facility goes down, you may lose all those records,” he said. He also stressed the importance of ensuring those records are kept current. Healthcare organizations should also be prepared with reserve funding against a possible rise in uncompensated care. “After a disaster where many people have lost everything financially, their ability to pay their health bills will be limited,” he said.
3. Perform an inventory of critical assets. Organizations should be prepared for the financial impact from the loss of these important assets. “If you are an academic health center, for example, you may have invaluable research assets, such as an irreplaceable cell line that has to be protected. So you might think about splitting samples and performing the research someplace else.”
Benjamin encourages health system leaders to think broadly and ask themselves about the extent to which they are covered for those assets. “If they go away, am I able to pay for my staff? Do I have enough reserves to pay salaries for people who may be funded on non-reimbursable dollars?”
4. Review your insurance coverage. Health systems should pull all the insurance policies and make sure they know what they’re covered for, what the limits of those coverages are, what are the exclusions and specifics for those coverages. But in a disaster, they also should be prepared for slow payment.
5. Avoid a loss of power. “We’ve learned a lot over the years about hospital design,” Benjamin said. “We know, for example, you don’t keep your generators in the basement in a flood zone, because they will flood. But even if you’re not in a flood zone, they might flood. A lot of the historical flood zones are changing.”
6. Have a contingency plan for patients with special needs. Health systems typically spend a lot of time thinking about what to do when the power is out in the ICU. But they also should think about maintaining care for people who are on life support in the community. Benjamin said facilities that perform kidney dialysis could bring patients in early for treatment if a storm is coming, and the facility might be out of power out for several days.
7. Consider your supply lines. One of the things learned through emergency preparedness discussions is that everybody has a list of suppliers, but it often turns out we all have the same supplier. “So if that supplier goes down, everybody goes down.”
Footnotes
a. Reese, E.C., “2020 vision: What to expect in healthcare finance over the next decade,” hfm, January. 2020.
b. NASA, “Scientific consensus: Earth’s climate is warming;” site last updated Feb. 20, 2020.
c. D’Angelo, C., “Interior secretary blames Congress for his inaction on climate change,” High Country News, May 9, 2019; and Feldman, S. and Lavelle, M., “Donald Trump’s Record on Climate Change,” Inside Climate News, Jan. 2, 2020.
d. A vector-borne disease is one that is transmitted to humans and other animals by a vector, which refers to mosquitos, ticks, fleas and other blood-feeding organisms.
e. SciLine, “Vector-borne diseases in the United States,” last updated April 15, 2019.
f. Blumenthal, D., and Seervai, S., “To be high performing, the U.S. health system will need to adapt to climate change,” To the Point, The Commonwealth Fund, April 18, 2018.
g. A CMS fact sheet notes U.S. national healthcare spending grew 4.6% to $3.6 trillion in 2018, or $11,172 per person, and accounted for 17.7% of gross domestic product. (The fact sheet was last modified on Dec. 5, 2019.)
h. Dettman, L., “The cost of climate change,” Public Health Newswire, July 25, 2019.





