4 crucial health system responses to the revenue impact of COVID-19


Hospital and health system financial performance has been devastated by the blindside hit from the COVID-19 pandemic. Recovery from the unexpected disappearance of hundreds of billions of dollars in patient care revenue in just a few short months will require both operating discipline and a dynamic approach to budgeting and managing payer relationships. It is imperative that organizations begin now to prepare for the ultimate financial impacts of the pandemic.
In the first three months after the COVID-19 pandemic struck, the typical U.S. hospital lost half its emergency visit volume, 70% of its surgical volume and 30% of its inpatient admissions. According to the American Hospital Association, the pandemic could end up causing $320 billion in hospital revenues to disappear in calendar year 2020. And two-thirds of hospital financial executives responding to a May 2020 Guidehouse/HFMA survey said they expect a 15% shortfall in annual revenues, with almost one-fifth of executives projecting a shortfall of 30% or more.
Healthcare organizations should prepare for the ultimate financial impacts of the pandemic, including the expected significant decline in commercial insured patients and the resulting increase in Medicaid, exchange and uninsured patients over the next few years by adopting a more aggressive financial management approach. (See the sidebars below for more about the impacts of COVID-19 on healthcare and the nation.)
4 strategies for dealing with the financial uncertainty
It seems clear that a post-COVID-19 health financing backlash is already upon us, requiring action by hospitals and health systems. Here are four key components of an effective strategy for health systems to implement.
1. Dynamic budgeting. If the COVID crisis has done anything, it has definitively ended the use of passive annual budgeting. With likely major swings both in payer mix and unit payments ahead, relying on 18-to-24-month-old revenue forecasts to set staffing levels has become dangerously ill-advised. It is imperative that hospital and health system C-suites use rolling forecasts of revenue mix and growth and continuously track revenue realization by payer class and contract. This approach is essential now due to the uncertain pace of “re-opening” amid COVID surges, but also will be even more essential in the next two years as employer-based insurance and public financing programs are hit hard by economic stresses.
2. Aggressive cost management. To drive improvement, organizations will need to work aggressively to reduce fixed costs and manage variable costs in real time, based on timely estimates of expected revenue.
Fixed costs, including corporate overhead of all types, vendor contracts and physician services contracts, must be reduced in response to reflect the reality of interrupted service volume and an uncertain recovery.
Variable expenses will need to be adjusted in real time to fit within the envelope of actual realized revenues. These expenses include not only clinical staffing, but also support staffing (housekeeping, food service), supplies and pharmaceuticals. As most CFOs and COOs know, many variable expenses masquerade as fixed costs. As one CFO of an investor-owned facility once told us, “In reality, there is no such thing as a fixed cost.” Converting fixed costs to variable as an operating philosophy will be key element in the painful re-adjustment process that will be required in response to the COVID-19 crisis.
3. A portfolio approach to managing payer contracts/relationships. Such an approach is essential for protecting revenue. One major unpleasant surprise for hospitals from the value-based contracting that followed Obamacare was a surge in denials, repricing and recategorization of services (e.g., reclassifying acute admissions as observation stays) that followed. Much of this surge was driven by automated prepayment claims reviews performed by artificial intelligence (AI) algorithms that incorporate machine learning. These reviews have profoundly affected not only Medicare Advantage (MA) and Medicaid contracts but also regular commercial contracts, where the involved carriers often are actually different divisions of the same large health plans.
As insurance carriers have experienced sharp reductions in their medical loss ratios (MLRs) as a result of providers’ suspension of elective care imposed by COVID-19, denial rates appear to have fallen. When insurer MLRs begin rising again, either due to a surge of COVID-19 claims or to resumption of elective care, it is realistic to expect another surge of machine-driven denials leading to renewed problems with revenue yield. Contract rates set on the basis of expected collections from patients are likely to be lower than adequate due to reduced patient payment of their share of the cost, resulting from COVID-19 job losses and exhausted family savings.
All these factors underscore the strong need for every hospital and health system to manage its contracts with payers as if they were a portfolio of risk. In this context, risk refers not only to “bonus-related” risk relative to cost and quality metrics, but also the core financial risk of adequate coverage of the hospital’s incurred expenses. For MA and managed Medicaid, both of which are likely to grow rapidly, the challenge is not merely to manage the contracts, but also to manage the healthcare delivered to enrollees and to improve their health by better addressing their disease risks. Important steps are to:
- Review the organization’s service line(s) and site of services in order to position the organization for sustained profitability. In particular, the line between allowable inpatient and outpatient services seems to be increasingly fluid and laden with cash flow risks.
- Continuously review the outside factor(s) that introduce risk to clinical volume (competition, disruptors, etc.).
Programmatic changes may be required as the organization moves through these steps to ensure effective use of its beds, technology and clinicians, including consolidating or eliminating duplication, training clinicians on optimal documentation, reducing waste in clinician time and ensuring effective communication with patients and families about their financial responsibilities.
Within this approach, the organization should implement processes within its revenue cycle to:
- Monitor payments for each contract.
- Identify the sources of negative variances and trends in same
- Aggressively pursue correction of those variances that are under your or your clinicians’ control.
- Optimize use of the EHR to automate as well as possible documentation of clinical conditions required for appropriate payment, and ensure integrity of claims to payers
- Intervene with the involved carrier as needed to ensure that they are complying with the terms and conditions of the contract
For health plans that persistently shortchange the hospital, or for whose covered lives the hospital receives inadequate payment, hospital executives should be prepared to terminate the contracts or dramatically alter contract terms at renewal.
4. Investment in growth of telehealth and telework. One pleasant surprise emerging from the COVID-19 crisis has been rapid acceptance and use by consumers of virtual visits with caregivers as a substitute for in-person visits. According to the Guidehouse/HFMA survey, telehealth volumes will have increased more than 300% in 2020 over 2019 levels. This expansion of volumes will be part of the new normal post-COVID.
Telehealth offers the potential of both enhancing revenue and reducing expenses. Telehealth can be particularly effective for:
- Answering consumer questions about the need for in-person care
- Receiving or adjusting patients’ medication requests
- Following up on post-surgical care
- Maintaining and strengthening primary care relationships
It is not unreasonable to expect that one-third to one-half of ambulatory visits could be managed virtually, thereby making it possible to reduce clinic space and staffing expenses.
Another pleasant surprise is how telework arrangements have gained acceptance among the hospital and health system staff. Virtual work arrangements seem likely to grow non-incrementally in the wake of the COVID crisis, with parallel opportunities to reduce office space, further reducing fixed expenses. An additional benefit is to the potential to reduce the amount of time consumed by often poorly managed in-person meetings. Being able to handle these functions virtually and, in some cases, asynchronously can save precious and expensive executive time, and markedly improve speed of decision-making and operating efficiency.}
The pandemic’s ongoing impact
COVID-19’s impact on providers’ finances is likely to stretch far beyond the end of 2020 into at least the two following calendar years. Health system finance leaders should prepare for the repercussions of the sudden violent economic downturn caused by COVID-19 on their payer mix and unit payments. Profound and volatile changes in hospital revenues will demand sharper analytics, near real-time revenue cycle management and more aggressive expense control if health system leaders are to regain control of their organizations’ financial destiny.
Beware the COVID-19 backlash
COVID-19 has resulted in perhaps $2 trillion in activity disappearing from a $21 trillion U.S. economy, more akin to a flash depression than a recession. The U.S. Department of Labor reported on Sept. 17 that, as of the end of August, more than 27 million people were receiving unemployment. And in July, the Urban Institute issued the following preliminary estimates for the more than 10 million workers who lost healthcare coverage with their jobs:
- Perhaps 30% will become uninsured and be unable to pay for needed care.
- One-third will be eligible for Medicaid
- One-third will be eligible for exchange-based coverage under Obamacare.
The actual uptake rates for Medicaid and exchange enrollment and the extent of growth in uncompensated care will depend on the severity of each state’s downturn.
Normally, it takes 18 months from the onset of a recession for hospital industry cash flow to be affected. The amount of structural damage that has occurred in the economy will determine the longer-term impact on the healthcare payment system. Hospitals budgeting for 2021, 2022 and perhaps 2023 will be indirectly but powerfully affected by how many businesses close permanently in the wake of COVID-19 and by how rapidly business returns to severely impacted sectors such as oil and gas, travel and entertainment, restaurants and food service, food processing, retailing and distribution.
COVID-19 state budget shortfalls could be largest on record
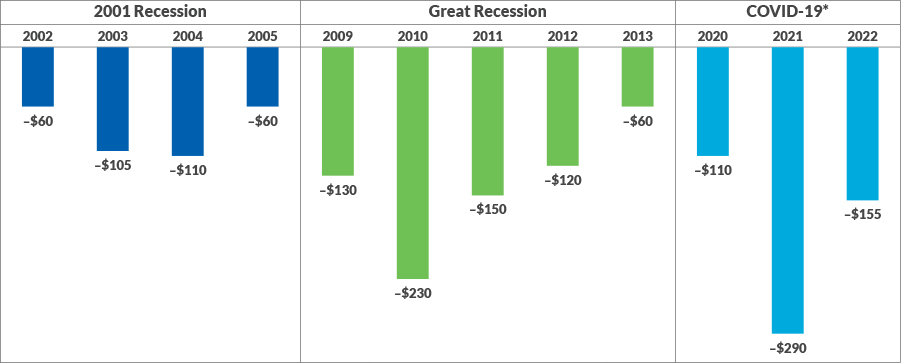
Total state budget shortfall in each fiscal year, in billions of 2020 dollars
Source: Center on Budget and Policy Priorities (CBPP), Pre-2014; CBPP Survey, 2020.
For the nine to 24-month window beyond the end of calendar 2020, it is reasonable to expect a significant decline in commercial insured patients and a resulting increase in Medicaid, exchange and uninsured patients. Medicare will continue expanding by about 2.5 million people a year as the younger half of the 76-million-person baby boom enrolls.
Moreover, collection rates from the substantial fraction of remaining commercial patients who have high-deductible plans are likely to deteriorate due to interrupted employment and family cash flow problems. The rise in so-called “self-pay” bad debts played a major role in the 39% drop in operating earnings hospitals experienced from 2015 to 2017 at the height of the economic boom. It is prudent to expect significant deterioration in both insured and uninsured patient self-pay collection rates.
Impact on Medicaid. The Medicaid program is likely to pose a special problem. Due to the Obamacare Medicaid Expansion, some states had a third or more of their citizens enrolled in Medicaid at the peak of the boom, and some 72.3 million total were enrolled at the end of April 2020. Before the COVID-19 financial crisis is resolved, a few states may end up with 40% or more of their citizens on Medicaid.
Medicaid is the balancing item in state budgets, amounting to more the 20% of general fund spending, on average, second only to education. Recent estimates show a shortfall of $55O billion in state budgets over the next three years. Unless Congress further enhances federal matching for state Medicaid funds, cuts in Medicaid funding are inevitable in 2021 and 2022.
Beyond COVID-19: Preparing for price transparency’s impact on payment rates and collections
In addition to responding to the revenue impact of COVID-19, hospitals and health systems must prepare for the new federal price transparency regulations, effective Jan. 1, 2021, which will exert pressure both on consumer payments and on payer negotiations. Public information about disparities in payment rates from payer to payer and facility to facility will massively complicate payer contract negotiations. Providers with high contract rates relative to market will need to justify their rates by promoting the value of the care, medical education and community service those rates help fund.
Other actions hospitals and health systems must undertake to ensure profitability in the wake of transparency include:
- Working with secondary commercial payers to improve inferior rates and terms
- Communicating more effectively with patients in advance about their share of the cost, and ensuring they receive value for what they spend
- Estimating the actual costs of care for patients more accurately and being prepared for consumer pressure to reduce those costs





