3 ways hospitals need to pivot their OR strategy in the wake of COVID-19

Elective surgery cancellations prompted by COVID-19 severely reduced hospital surgery volumes during the spring 2020 lockdown. Because the operating room (OR) can generate up to 70% of a hospital’s margin, these volume declines have erased the operating margin of most hospitals and health systems.
Equally concerning is the recent spike in COVID-19 cases, which has led to further surgery restrictions. While a vaccine has been approved and the vaccination of frontline providers has begun, COVID-19 infections and hospitalizations are expected to increase through the winter. Elective surgeries are once again being cancelled, and hospital financial performance is continuing to deteriorate.
In responding to these financial challenges, many hospital leaders have focused largely on protecting traditional OR service lines and preserving higher payment for hospital-based procedures. The problem is that the traditional hospital surgery market was shrinking before the pandemic, and COVID-19 only accelerated its decline.
Hospitals cannot shrink their way to growth. To maintain procedural revenue in the years ahead, hospital leaders require a new surgical services strategy. Current needs and longstanding trends suggest the best approach is to adopt an “ambulatory first” strategy that pivots the organization’s focus to outpatient access, an exemplary patient experience and enhanced operational efficiency.
1. Pivot to outpatient care
Surgical care has been migrating from the inpatient setting to outpatient clinics for decades.a Meanwhile, hospital share of the outpatient surgery market has been shrinking — from 59% in 2005 to approximately 40% today.b
Most hospitals have been insulated from this trend by a moat of high-revenue procedures that can only be performed in an inpatient OR. They have also been buoyed by higher reimbursement for ambulatory procedures performed in a hospital outpatient surgery department (HOPD). However, this favorable pay differential is steadily decreasing, and CMS recently proposed to eliminate the Medicare “inpatient only” list.c
Inpatient surgery will continue to be an important service line in the years ahead, but it can no longer anchor surgical services revenue. Going forward, outpatient surgery must become the core of perioperative strategy.
For hospital leaders, the first priority is to develop a wider network of ambulatory surgery delivery sites. There are two broad options.
Build an ambulatory network. The first option is to focus on developing a network of new ambulatory surgery centers (ASCs). A build strategy requires a significant investment, but it provides the opportunity to start with a blank slate and create a patient-focused and highly efficient ambulatory network.
Buy into existing centers. The second option is to acquire existing ASCs, typically from surgeon owners who are near retirement. This approach is less capital-intensive than building from scratch and offers a faster ROI. Strategically, it can allow an organization to secure existing ASC volume before competing hospitals do.
As they weigh these options, finance leaders should be aware of a less-known trend. In several markets, venture capital funds are actively acquiring surgeon-owned ASCs in profitable niches such as orthopedic surgery and urology. These investors can pose a competitive threat for hospitals. However, they also represent an opportunity. Many funds are open to partnering with hospitals to develop ASCs, thereby affording the hospitals the financial leverage they need to quickly grow an outpatient surgery network.
2. Pivot to patient experience
In the traditional view, the focus of ORs is simply to deliver surgical procedures: After the patient undergoes the procedure, recovers and is discharged, the hospital’s work is done. By contrast, in the surgical services strategy of the future, the ultimate objective should be to deliver an excellent surgical experience for patients.
An excellent patient experience is essential for maximizing value-based payment. It also is critical to competing effectively in the consumer-oriented outpatient surgery market. Delivering an unparalleled patient experience requires the following elements.
A focus on outcomes. Clear functional and clinical goals are essential to designing a well-coordinated clinical pathway for surgery patients. For example, outcome targets for an orthopedic surgery center might include activities-of-daily-living (ADL) metrics at three, six and 12 months. With these goals in place, surgery leaders can work to ensure every component of care (e.g., scheduling, pre-surgical preparation, intraoperative care, discharge processes and rehabilitation) contributes to an excellent patient outcome and experience.
Personal attention. Patients come to surgery not only with a clinical need but also with personal concerns. To create an excellent patient experience, ASCs should have a process in place that emphasizes at every step customer service, patient communication and patient/family convenience. For instance, an ASC might offer same-day scheduling for urgent needs such as certain pain procedures.
Digital tools. Remote healthcare got a boost during COVID-19, and it has proven to be very popular with patients. ASCs should build on this foundation. Many preoperative and postoperative interactions can be converted to video. Some ASCs and inpatient ORs also are using smartphone apps to communicate with surgery patients about scheduling, coordinate pre-surgical testing and communicate pre-procedure instructions.
New service lines. New outpatient procedures are emerging that deliver excellent patient outcomes and have the potential to expand the elective surgery market. For example, cardiology and spine procedures are increasingly being performed on an ambulatory basis. Finance leaders should maintain an awareness of the significant opportunities these high-volume, high-margin procedures present for ASC growth, and enlist the help of clinicians to develop these new service lines. Outpatient service line strategy also can target niches such as workers’ compensation, dermatology and plastic surgery.
New facility strategy. Patient convenience is an integral part of the ASC concept. Leading organizations are now building on that concept with the integrated surgical campus, in which an outpatient surgery center is co-located with ancillary services such as diagnostic imaging and radiation therapy, supporting clinics such as PT and pain management, and physician offices. For patients, this strategy consolidates the surgery experience into a single convenient campus, which is typically located near high-traffic retail.
Developing an integrated surgical campus
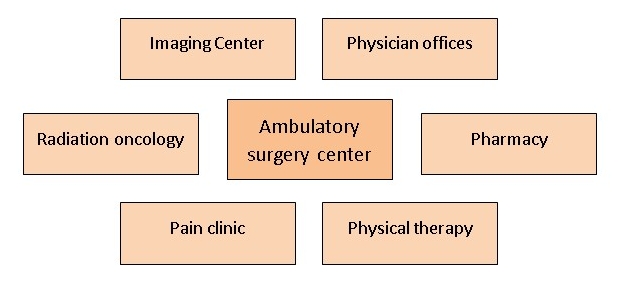
Some healthcare organizations are consolidating the outpatient surgery experience into a single convenient campus that provides a full spectrum of services.
Source: Surgical Directions, 2020
3. Pivot to efficiency
Although outpatient surgery payment rates are increasing, they are still significantly below inpatient rates. Thus, as hospitals pivot to an ambulatory strategy, finance leaders must pay strict attention to the margin.
The biggest opportunity right now is in capacity utilization. Most OR management teams are content if they can get primetime utilization above 60%. But even in this “best-case scenario,” more than one-third of expensive OR capacity goes unused.
The following steps are key to addressing this waste, optimizing the OR schedule and improving efficiency overall.
Use predictive analytics. Currently, OR managers use historical averages and utilization peaks to estimate room needs. As a result, the OR schedule tends to be over-staffed but also is vulnerable to utilization surges. ORs can use predictive analytics to design a room schedule that more tightly aligns demand with capacity. Such an approach requires three broad steps:
- Obtain at least 12 months of data on room utilization by day of week and hour of day.
- Use the data to calculate (to 95% probability) the number of rooms running each hour.
- Use the results to generate a heat map of OR demand.
Using predictive analytics to optimize the OR cost structure
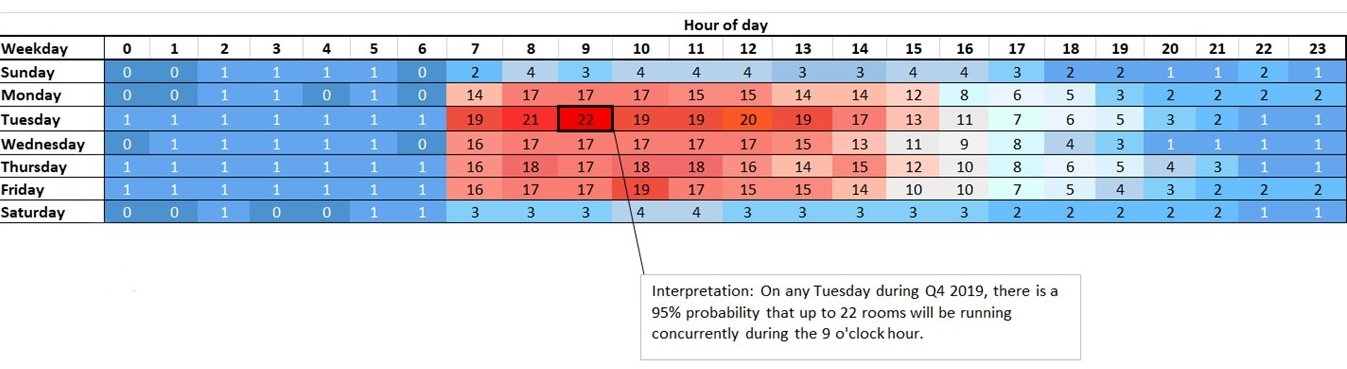
This heatmap displays the probability of concurrent rooms running in a hospital surgery department by day and hour. Staffing for probability allows an OR to streamline its staffing model.
Source: Surgical Directions, 2020
A utilization heat map provides an accurate picture of the ebb and flow of demand in a hospital surgery department or outpatient surgery center.
Engage physician leadership. Even with the advantages provided by predictive analytics, OR leaders still need to work with surgeons to tailor a block schedule that supports strong utilization. The key is to establish a surgical services executive committee (SSEC), a physicians-led governance body for surgical services.
An SSEC typically comprises five or more active surgeons and anesthesiologists, with additional representation from nursing leadership and hospital administration. The committee’s purpose is to allow surgeons — the principal customers of surgical services — to take responsibility for optimizing the OR’s efficiency. Many hospital executives are uncomfortable with this idea initially because they fear an SSEC will establish rules and processes that benefit physicians but negatively impact the hospital. However, t20 years of experience with this approach has proven that a well-functioning SSEC can quickly allay these concerns by boosting OR efficiency and financial performance.
Ideally, SSEC member physicians should be respected for their clinical skills and have a demonstrated ability to lead an organization through change. SSEC members should also be clinically active, know how the OR functions and have a vision of what needs to change to improve OR performance.
A strong SSEC can work with the surgeon staff to design a block schedule that provides excellent access while allowing the OR to avoid opening unneeded rooms. An SSEC can also play a key role in pivoting to an ambulatory strategy. In a setting where most systems are designed to accommodate inpatient surgery, the SSEC can help establish a culture more compatible with the needs of ambulatory patients and their surgeons. For example, committee members can develop systems for pre-surgical phone contact with patients to explain what to expect the day of surgery and through recovery. The committee also can help create an ambulatory block schedule that ensures patients are never bumped or delayed to accommodate emergencies.
When surgeons govern ASC operations, they typically create an efficient working environment. The surgeons on an SSEC are motivated to achieve such an outcome because they see the benefits for themselves and their peers, including the ability to perform more cases per day with fewer frustrations. They also recognize the likelihood that a well-run ASC or ambulatory network will become the provider of choice for surgeons in the local market.
Start with short-term plan
The pivots described here cannot be achieved overnight. Most hospitals therefore need a short-term plan to accommodate the volume surges after COVID-19 begins to subside. A solid short-term capacity-building plan can dovetail with long-term efforts. Key steps for such a strategy are described in the sidebar below: “5 key elements for launching the surgical services pivot to ambulatory care.”
Maintain the long-term view
An ambulatory-first strategy for surgical services offers several long-term advantages. In the context of COVID-19, distributed care sites could help hospitals become more resilient in future pandemics. Evidence shows that patients feel safer in ASCs while they remain reluctant to receive care in the main hospital’s OR.
A strong ambulatory surgery strategy also can promote the principles of value-based payment by helping hospitals improve outcomes, increase patient satisfaction, control costs and maintain a strong operating margin. Ultimately, such a strategic pivot can enable hospitals to reduce their dependence on a shrinking market and achieve real growth in surgical services.
Footnotes
a Blasco, T.A., The hospital executive’s guide to ASC expansion strategy, Surgical Directions, September 2019.
b Bill Frack, B., Williamson, J., and Grabenstatter, K., “Ambulatory surgery centers: becoming big business,” L.E.K. Consulting, Executive Insights, April 17, 2017.
c CMS, “Medicare Program: Hospital Outpatient Prospective Payment And Ambulatory Surgical Center Payment Systems And Quality Reporting Programs,” Federal Register, Aug. 12, 2020.
5 key elements for launching the surgical services pivot to ambulatory care
Developing a post-COVID surge plan should begin with the following basic steps, which can set the stage for the long-term shift of surgical services to the outpatient arena.
Capture case backlog data. The operating room (OR) management team should work with surgeon offices individually to identify cancelled and delayed cases and estimate the total case backlog. They should capture information not only on procedures but also on patient acuity, patient health status and payer mix.
Use surgeon case time data. One to two years of historical data should be captured to calculate the average case time per procedure by each surgeon. Case times can be widely variable, so this information is essential for accurately forecasting room needs.
Analyze OR capacity and utilization. Use a heat map process, as outlined above, to identify utilization patterns across all OR and ambulatory surgical center (ASC) sites. Overlay the current surgeon block schedule and look for opportunities to consolidate block time for under-utilizing surgeons. Also identify any equipment constraints (for example, the availability of C-arms) that could affect throughput for specific specialties and procedures.
Develop capacity expansion options. Some ORs may need to absorb a significant case backlog. One option is to schedule additional weekday blocks in the late afternoon and evening. Another is to organize specialty-specific weekend blocks. For example, a 10-hour Saturday block for hip replacement (with optimized setup and staffing) could allow an efficient surgeon to perform up to eight procedures in one day.
Create a case prioritization algorithm. To prioritize backlog cases for scheduling, the first filter should obviously be patient acuity. However, OR leaders also should prioritize cases by contribution margin. Individual volumes also should be balanced to ensure every surgeon can make acceptable progress on his or her backlog.
Although such an algorithm can go a long way toward mapping out an efficient OR schedule for the coming months, surgeon leaders will need to fine-tune all scheduling decisions. Again, a well-designed surgical services executive committee (SSEC) can effectively work through the surgeon issues that are nearly impossible for hospital executive to resolve alone.





