Why optimizing the patient experience should be on every C-suite leader’s radar
Jason Wolf, president and CEO of The Beryl Institute, knows from personal experience how easily a healthcare organization can lose a customer. A few years ago, his wife was mistakenly billed for a $25 copay that she already paid, and then the account was fast-tracked into collections. Despite receiving excellent clinical care, his wife vowed never to return to the organization because the experience was so frustrating.
Wolf says such stories should rattle CFOs and other C-suite leaders who do not recognize the importance of the patient experience, which The Beryl Institute defines as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.”
Often, it is the bookends of patients’ clinical experiences — what happens before they enter and after they leave the healthcare setting — that have the most impact on their satisfaction, Wolf says.
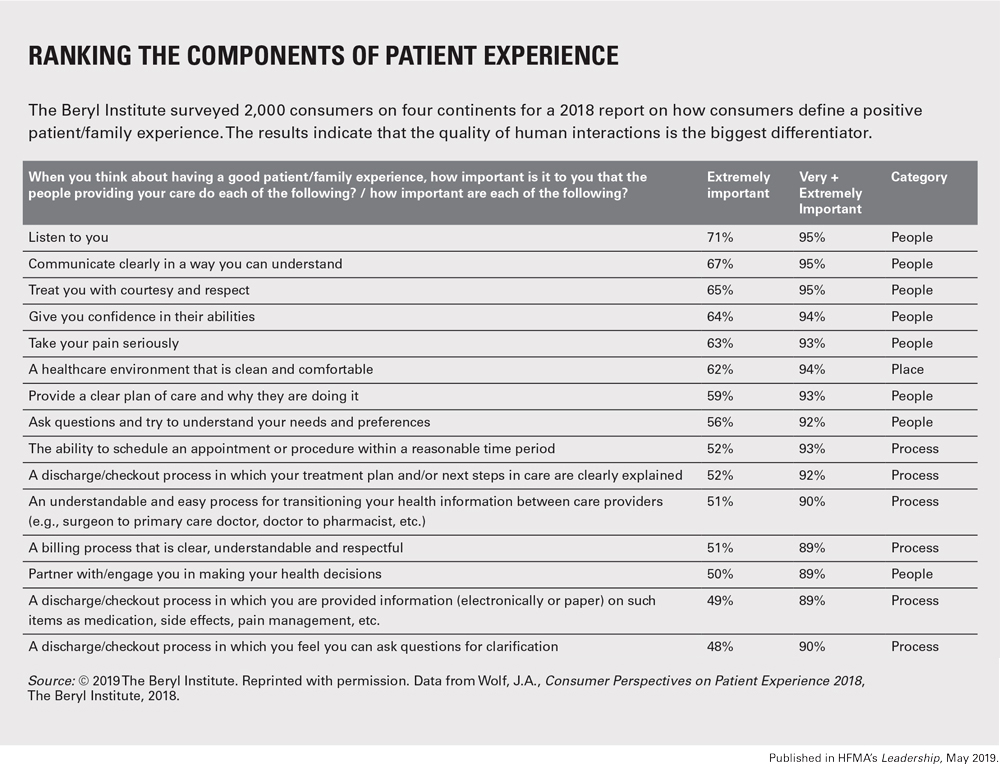
In The Beryl Institute’s 2018 study of consumer perspectives on the patient experience, nearly 90% of the 2,000 respondents said having a clear, understandable and respectful billing process was extremely or very important to their experience. Also important were easy access, clear discharge instructions and respectful communications.
The ripple effects of the patient experience
Today, most C-suite and senior finance leaders can quantify how much payment is at risk based on their HCAHPS survey scores. Yet it’s a mistake for leaders to view the patient experience purely in that context, Wolf says.
“We have to look at the broader ripple effects of the experience we create in our organization for the true impact of our efforts and investment,” he says. Although The Beryl Institute study found that consumers recall positive experiences over negative experiences, patients also said they share their experience with others regardless. And because consumers say the recommendations they receive from families and friends are the most important factor in their decision making, how patients experience their care should be top of mind for C-suite leaders.
Wolf issues this warning to leaders: If you fail to invest in the patient experience, you may lose potential customers to other organizations that can deliver what patients want, expect and deserve.
The evolving role of chief experience officer
In response to the rising tide of consumerism, about 65% to 70% of healthcare organizations have designated a senior leader who is responsible for the patient experience, Wolf says. Not all have the title of chief experience officer (CXO). Instead, they may have titles such as system director of experience or vice president of culture and experience.
Reporting structures also differ widely. Some patient experience leaders are considered part of the C-suite and report to the CEO, while others may be part of the quality department or report to the CNO or COO. Additionally, only about a third of these leaders are 100% focused on the patient experience.
Regardless of title, patient experience leaders can play valuable roles. They can help ensure that other C-suite leaders consider the patient experience as part of their organization’s growth strategy, capital investments, new construction, technology and staffing practices, Wolf says.
“Having a voice continually present or directly connected to the C-suite is vital to ensure this conversation isn’t just about tactics or achieving survey scores,” he says. “It is about having a fundamental strategy that integrates people and processes behind how you provide care, how you market and brand your organization, how you build your access and revenue cycle processes, and how you ensure excellence in care.”
How one hospital creates accountability for the patient experience
Jerry Mansfield, PhD, RN, is the first dual executive chief nursing officer and chief patient experience officer at MUSC Health, the clinical enterprise of the Medical University of South Carolina (MUSC). The health system’s hospital, MUSC Medical Center, has earned a four-star rating for the patient experience, according to the Hospital Compare website.
As part of his role, Mansfield meets regularly with his C-suite colleagues, including the CFO, to discuss how the patient experience affects growth, patient and family retention in the system, and repeat business — all of which can influence market share.
“If patients don’t have a great experience and they won’t recommend us to family and friends, we won’t see the volumes that we need in both our inpatient and outpatient settings,” he says. “We also have payers that are offering incentives if we outperform our peers in the patient experience. Last year, we left a significant amount of money from our major payer because we were just shy of the 85th percentile in patient experience scores.”
Across MUSC Health, leaders now accept the patient experience as a key performance metric, in part because the C-suite has made it a priority. “If the C-suite is not aligned in that perspective, it can create a struggle because people can deflect their level of accountability on impacting the patient experience,” says Mansfield (pictured).

To help drive accountability at every level, each leader at MUSC Health from the C-suite on down has adopted a patient experience goal for FY20. At the organizational level, targets are set each fiscal year for “top-box” scores, which represent the most positive response on HCAHPS survey items. Similarly, targets are set for the ambulatory, perioperative and procedural areas.
Nonclinical leaders will be asked in FY20 to take an organizational target most applicable to their potential to influence the patient perception. For example, billing/collections staff who manage outpatient accounts can take the ambulatory organizational patient experience target.
What CFOs can do to improve the patient experience
Wolf says CFOs can help other senior leaders by using cost-benefit modeling to assess which patient experience initiatives to support. Just as important, they can help reinforce the importance of the patient experience and the framework it provides in integrating key efforts around quality, safety and service.
“The CFO can shift the thought process of the organization to realize this is a true investment for success,” Wolf says, “not a cost that is a burden on the operations of the organization.”
Read more
For more examples of how hospitals are improving the patient experience, see:





