Why autonomous coding is having a moment in healthcare
Sponsored by AGS Health

Autonomous coding — coding powered by artificial intelligence (AI) — is emerging as a powerful tool for eliminating the administrative strain and error-prone processes surrounding manual coding in healthcare organizations.
It’s an approach that offers strong potential to increase productivity while reducing denials, missed charges and low-risk scores. It also helps providers make critical decisions faster.
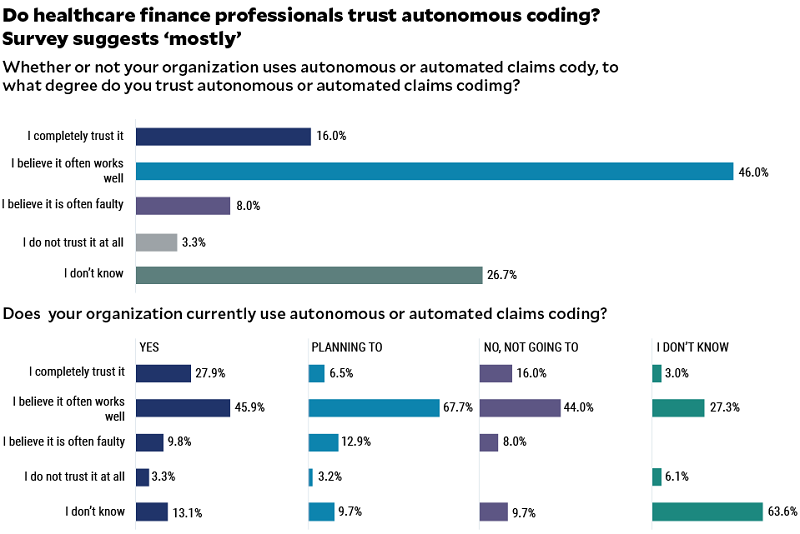
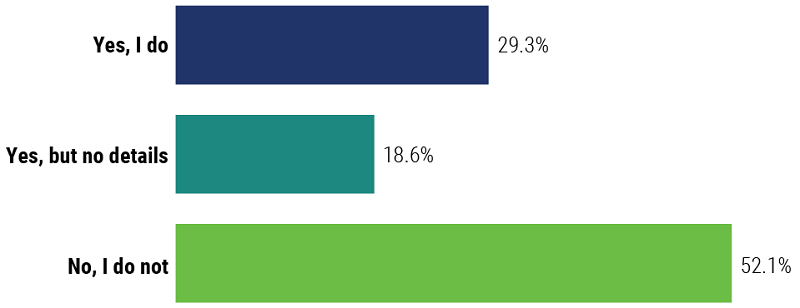
But while 60% of healthcare organizations surveyed during the 2023 HFMA Annual Conference said they either use autonomous coding or plan to, just over half of healthcare finance professionals surveyed (52%) responded that they still don’t know what autonomous coding is (see the exhibit on next page). Moreover, slightly more than one out of four aren’t sure whether to trust it, the survey shows.
“There is clearly a need for more education around what autonomous coding is and what it can do — and in what instances,” says Emily Bonham, senior vice president of Product Management for AGS Health. “Overcoming this knowledge gap will be essential to driving adoption, especially in specialties like radiology and emergency care, where autonomous coding drives more accurate and more efficient billing and reimbursement.”
It’s one reason healthcare professionals whose organizations use autonomous coding or are planning to have higher levels of trust — with some going so far as to say they trust it completely — than those that aren’t yet planning to adopt it. Closing the trust gap will be critical to accelerating use cases for autonomous coding in healthcare and improving the quality of documentation to support reimbursement.
The promise of autonomous coding for revenue cycle
When it comes to autonomous coding, there are several benefits:
- Eliminates the potential for human-introduced errors that result in missing reimbursement opportunities, backlogs, delays and claims errors.
- Elevates coders by transitioning them into the role of auditor.
- Understands what it does not know — and flags those charts for human review.
- Completes charts in seconds and the full process in minutes.
- Pushes accuracy levels to near-perfect percentages.
Source: The Evolution of Coding: Understanding How Technology is Assisting Us, AGS Health, https://www.agshealth.com/wp-content/uploads/2022/05/Whitepaper-The-Evolution-of-Coding.pdf.
The move toward autonomous coding
Accuracy in medical coding ensures claims for patient care can be processed efficiently and without the need for rework. This enables patients to receive the care they need, when they need it, at the appropriate location for care. It also protects an organization’s financial health, which supports its ability to provide high-quality care.
However, the increasingly complex nature of coding has led to significant growth in coding-related denials and revenue leakage. And while nearly two-thirds of claims denied due to medical coding errors or questions are recoverable, the costs associated with claim reprocessing, payment and reconciliation often become an overwhelming financial and resource burden. As a result, nearly 65% of all denied claims are never reworked.
Coding powered by AI — known as autonomous or automated coding — empowers healthcare revenue cycle teams to navigate the complexities of medical coding. It’s a solution that leverages technologies such as machine learning (ML) and natural language processing (NLP) to make code assignments, resulting in cleaner claims and reduced revenue losses for hospitals and healthcare systems. When a review of the claim suggests manual intervention is needed — a scenario that typically affects a minority share of claims — this technology matches coders with specific types of charts according to their skill level and area of expertise.
AGS Health commissioned this survey during the HFMA Annual Conference to determine the extent to which autonomous coding is taking hold in the healthcare industry. It also sought to pinpoint the value hospitals and health systems are gaining from a tech-enabled approach to coding and the barriers that stand in the way of implementation.
Among the 451 healthcare finance professionals surveyed — two-thirds of whom work in provider organizations — nearly 48% knew what autonomous or automated coding is, although 18% could not speak about it in detail. Among providers that do not yet incorporate autonomous coding into revenue cycle workflows, 20% plan to do so, and half of this segment plans to adopt a solution within six to 12 months.
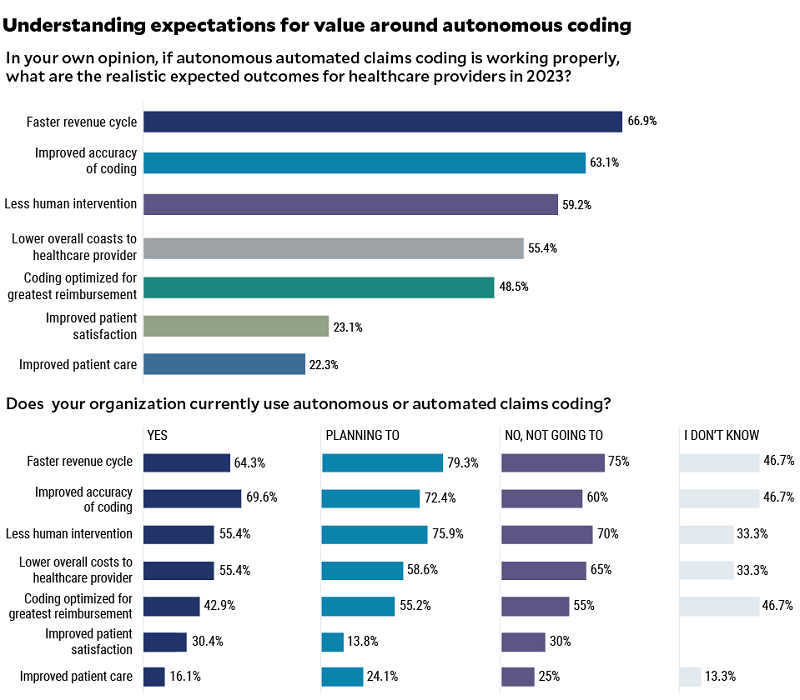
But even among those whose organizations already rely on autonomous coding, expectations for value vary. For example, nearly 70% point to improved accuracy of coding as an expected outcome, even though accuracy is one of the main selling points for investing in an automated coding solution. Fifty-five percent cite reduced need for human intervention in coding as a benefit, yet the ability to reduce demands on humans in the most labor-intensive aspect of healthcare revenue cycle is one of autonomous coding’s biggest strengths.
“Those who are planning to make the move to autonomous coding do have expectations of good results. They just don’t know how good those results are going to be yet,” Bonham said. Meanwhile, among respondents whose organizations currently use autonomous coding, “We believe there’s a misunderstanding around what autonomous coding is able to do,” she said. “For example, some people think autonomous coding should be applied across the entire organization, but that level of capability is still maturing with varying degrees of success depending on specialty. This is a nascent technology that is rapidly maturing.”
Nearly half of healthcare professionals aren’t strangers to autonomous coding
Do you know what autonomous or automated claims coding is?
Achieving optimal value from autonomous coding
The market for autonomous coding is expected to reach $88 billion by 2030, up from $35 billion in 2022. That’s not surprising given that coding is the most labor-intensive aspect of revenue cycle operations and the most vital to reimbursement. At a time when workforce shortages are putting a strain on revenue cycle resources, one recent survey found revenue cycle automation ranks as a top area for technology investment this year.
Yet there are barriers to autonomous coding adoption, a poll taken during an AGS Health webinar shows. These include:
- Budget/cost: 32%
- Previous investment in computer-assisted coding: 21%
- The belief that coders do more than coding, such as abstraction: 68%
- Insistence that partial automation is not enough: 11%
“We need to overcome the mindset that healthcare revenue cycle departments can’t afford to invest in autonomous coding,” said Thomas Thatapudi, CIO, AGS Health. Given that three out of four healthcare leaders plan to hire more coders and revenue cycle staff, “autonomous coding offers a way to solidify coding expertise by applying AI to all but the most specialized claims. This generates tremendous productivity gains, reducing days in accounts receivable [A/R]. In fact, one pilot program demonstrated a 700% increase in productivity by applying autonomous coding.”
But a plug-and-play approach by itself will not deliver the value organizations seek. Keep the following considerations in mind.
Understand that there will always be a need for human coders. “You will always need human coders to train the AI model for autonomous coding,” Thatapudi said. “The amount of coding that is performed manually will be reduced, but healthcare organizations still need coders to monitor the AI output. Just as an airplane might have an autopilot feature, you wouldn’t fly a plane without a pilot present. The same is true for autonomous coding.”
Determine how well the autonomous coding solution will integrate with existing systems. Among survey respondents, integration with existing systems was cited as the second-highest factor in selecting an autonomous coding solution, just behind accuracy. “This reflects the importance of healthcare system interoperability when making decisions around solutions such as this,” Bonham said.
Define benchmarks for measuring the quality of autonomous coding. These include the percentage reduction in denials (expect a 25% to 50% reduction in coding-related denials), decreased days in A/R (typically three to five days fewer after six months of implementation), as well as accuracy rates, which can reach 85% to 95% or higher.
Ensure your organization can personalize its approach to edits. “The right vendor will allow you to create custom edits based on what your team is seeing from recent audits,” Thatapudi said.
Request the ability to dig deeper into audit data. Make sure the vendor will allow your team to audit specific events, combinations of codes and more to better understand performance. “That’s one of the biggest gaps in the industry right now: You cannot control the audit,” Thatapudi said. “Revenue cycle leaders should be able to decide what types of audits they would like to perform and configure their systems to perform those audits.”
Taking the leap
It’s clear that autonomous coding is having a moment in healthcare, with a significant proportion of healthcare finance professionals aware of its potential. Moreover, healthcare leaders are ready to explore automation in the revenue cycle. The key to more widespread adoption will be education on what to expect from autonomous coding, how to deploy it and ways to optimize an approach. Only then can the healthcare industry build trust in this tool among the teams who need it most.
About AGS Health
AGS Health is more than a revenue cycle management company—we’re a strategic partner for growth. With expert services complemented by AI-enabled technologies and high-touch support, AGS Health is the premier revenue cycle partner for leading health systems, physician groups, and academic medical centers in the U.S. With expert insight into modern revenue cycle practices, we pair cutting-edge technology with college-educated, trained RCM experts to help customers achieve a high-performance revenue cycle to optimize workflows, maintain compliance, prevent revenue leakage, and grow their topline. AGS Health employs more than 12,000 team members globally and partners with over 140 customers across a variety of care settings, specialties, and billing systems.
This published piece is provided solely for informational purposes. HFMA does not endorse the published material or warrant or guarantee its accuracy. The statements and opinions by participants are those of the participants and not those of HFMA. References to commercial manufacturers, vendors, products, or services that may appear do not constitute endorsements by HFMA.





