The economics of a telehealth visit: A time-based study at Penn Medicine

Neil Ravitz, MBA

Sean Looby, MHA

Calvin Jordan, MBA

Andrew Kanoff, MHA
Should a healthcare organization reasonably expect to be paid the same or nearly the same rate for delivering telemedicine services as it receives for comparable services delivered in-house? Answering this question is critical to ensuring telemedicine’s future profitability.
At the onset of the COVID-19 pandemic, payers, providers and patients all embraced telehealth seemingly overnight, regardless of their stance on its use before the pandemic.
Since then, however, the spike in the use of telemedicine services has generally subsided, and providers have been left with many unanswered questions about the long-term economic viability of telemedicine services.
From the patient’s perspective, the continued availability of telemedicine services used appropriately and in place of an in-person visit is a clear win: Patients can receive care in the comfort of their home while avoiding travel-related costs and spending less time away from family, work or other obligations.
But for providers, the picture is less clear from a payment perspective. Some argue that telemedicine can be efficiently delivered at a cost lower than the cost for in-person services. They suggest less physical space and staff support are required for telehealth services, therefore warranting lesser payment rates.
Others suggest the incremental resources and associated costs including electronic platforms, work-from-home costs and efforts required to help patients cross into the digital world have increased the cost structure and negated any potential savings.
Research needed
The problem is that in the telemedicine world, physician groups and health systems have limited data to make a case with government or commercial payers regarding how they should be paid for their services. At Penn Medicine in Philadelphia, we recognized that resolving this ongoing debate requires new research to more deeply understand the optimal use, coverage and payment for telemedicine visits in a post-pandemic world.
Thus far, studies that have pointed to savings from telemedicine in lieu of in-person services have generally focused on the redirection of services away from high-cost areas such as the emergency department. But to truly begin to understand the relative costs of delivering telemedicine services versus in-person services, studies must consider other factors, including the actual staffing differences required to coordinate and deliver care.
This realization spurred the leadership team of Penn Medicine’s Department of Orthopaedics to undertake a study of the telemedicine services it delivers, looking at all facets of how an inperson visit is organized, delivered and reimbursed compared with a telemedicine visit. We focused on the staffing aspects of the cost structure, the piece most under the department’s control, but also considered other quantifiable revenue and expense factors.a
Comparative cost of staff support
The leadership team in the Department of Orthopaedic Surgery performed a time study to measure the staff effort necessary to support an in-person visit as compared with a telemedicine visit. We began by dissecting a visit into its component parts, beginning with appointment scheduling and pre-visit elements, and ending with post-visit elements, including scheduling of any required follow-up visits or surgeries.
This approach allowed us to understand which elements are consistent and require an equal effort for in-person and telemedicine visits, and which elements involve differences in process and effort.
We then focused our time study on the elements that differed and examined the actual differences in staff time and effort required for each task. The complete set of visit components is shown in the exhibit below, with the highlighted blue rows representing the key elements where processes differ between in-person and telemedicine visits.
Visit progression components: In-person versus telemedicine
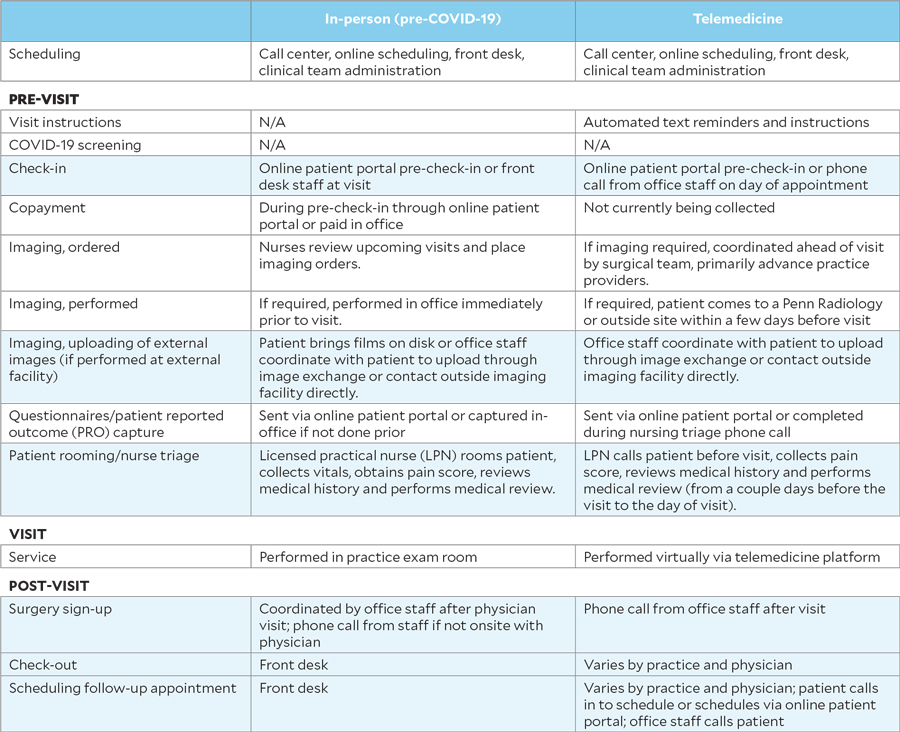
The time study portion of the study performed by Penn Medicine’s Department of Orthopaedics looked at differences in staff time and effort for each task included in an in-person visit compared with a telemedicine visit. The highlighted blue rows represent key elements where processes differ between in-person and telemedicine visits.
Our study focused on two of our busiest outpatient practice locations in downtown Philadelphia, which have a diverse patient population. The study was conducted during November and December 2020, with staff documenting the amount of time spent on each task for more than 700 visits. During this time, the overall telemedicine use rate in these practices was 7%. We computed average staff time for each task and used average staff hourly rates to compute the cost of the incremental time. The examined tasks, differences in staff time to complete and overall staff-expense-per-visit impact are summarized in the exhibit below. Although the incremental numbers listed may seem small, the impact becomes clear when one considers the volume of visits.
Comparison of select tasks and average time to complete (minutes)
Select Task | In-person | Telemedicine | Telemedicine incremental |
| Front desk check-in | 2.5 | 4.0 | 1.5 |
| Imaging support* | 1.0 | 1.0 | |
| Patient rooming/nurse triage | 5.0 | 6.0 | 1.0 |
| Check-out/surgery sign-up/follow-up scheduling | 2.0 | 3.0 | 1.0 |
| Subtotal | 9.5 | 14.0 | 4.5 |
| Incremental staff cost per visit (compensation and benefits)† | $2.40 |
* Telemedicine external imaging support estimated at an additional 20 minutes per patient for 5% of patients (20 minutes × 5% = 1 minute, on average)
† Weighted average inclusive of the following roles: patient service associate, licensed practical nurse, patient care
Average staff time for each task was computed, and average staff hourly rates were used to compute the cost of the incremental time for examined tasks. This exhibit summarizes differences in staff time to complete tasks and overall staff-expense-per-visit impact. Although the incremental numbers listed may seem small, the impact becomes clear when one considers the volume of visits.
Impacts of other factors
We also assessed the impact of three additional factors on the revenue or expense differences between in-person visits and telemedicine visits:
- The technology cost of the telemedicine platform
- Performance of telemedicine visits in a hospital outpatient department (HOPD) setting
- Cost savings from using existing facilities
Technology cost = a modest expense increase. We broke down the cost of the telemedicine platforms into a per-visit cost based on our total cost incurred divided by total telemedicine visits, across the entire health system. As a large health system conducting over 50,000 telemedicine visits per month during this period, we found this cost was nominal on a per-visit basis. But it could be considerably larger for smaller organizations and independent practices. We also were able to keep cost down by flexing corporate FTEs to focus solely on implementation of the telemedicine platforms.
Use of HOPDs as a setting for telemedicine = a revenue decrease. Several of Penn Medicine’s sites for telemedicine services are licensed as HOPD practices. Telemedicine payment for Medicare patients does not account for HOPD status, resulting in a lesser payment for a telemedicine visit.
We calculated this impact using the following formula:
Average reduction in Medicare payment for telemedicine at HOPD practice × % of total visits for Medicare patients at HOPD sites
An important consideration is that the reduced payment applies only to health-systemowned practices with HOPD licensed sites, and only for patients covered by Medicare or other applicable payers. It could be affected by how providers bill for their services, potential Medicare billing updates and any future Medicare reimbursement changes for siteneutral payments.
Facility-related cost saving = reduced expense. The savings stems from not needing to rent additional physical space to treat more patients via telemedicine. The premise was that if no additional facility expenses would be incurred or allocated by delivering telemedicine services, any rent expense associated with incremental telehealth visits, not counting those that simply replaced in-person visits, would be spread over a larger visit base and reduce overall expense per visit.
We calculated this effect using the following formula:
Total rent expense ÷ Total visits = Rent expense per visit
We assumed savings would increase at higher levels of telemedicine use and that current space costs were fixed.
Overall findings
We quantified the financial impact of all these factors on a per-visit basis, and then extrapolated the results to estimate the overall net impact on our entire Orthopaedic Surgery enterprise.b The estimated net impacts based on our current telemedicine use rate as well as higher use rates are shown in the financial model below. This model is intended only to quantify the financial impact of telemedicine as an alternative to in-person visits, with total visit volume remaining the same. It does not consider the impact of utilizing telemedicine to grow incrementally above current visit volumes, which would require additional study. Our analysis forced a deeper level of understanding and thinking around telemedicine, allowing us to examine factors that are under our control as well as those that are not.
Telemedicine financial impact model*
Telemedicine use rate | |||||
| Current/actual | 15% | 30% | Code | Calculation | |
| Total annual visit volume | 140,000 | 140,000 | 140,000 | A | |
| Telemedicine use rate (% of total visits) | 7% | 15% | 30% | B | |
| Telemedicine visit volume | 9,800 | 21,000 | 42,000 | C | A × B |
Incremental staff cost | |||||
| Incremental staff cost per visit | $2.40 | $2.40 | $2.40 | D | |
| Total incremental staff cost impact | -$23,520 | -$50,400 | -$100,800 | E | C × D |
Telemedicine technology platform cost | |||||
| Expense per visit | $0.32 | $0.32 | $0.32 | F | |
| Total incremental technology cost impact | -$3,136 | -$6,720 | -$13,440 | G | C × F |
Hospital outpatient department (HOPD) impact | |||||
| Percentage of total visits at HOPD sites from Medicare patients | 20% | 20% | 20% | H | |
| Average HOPD revenue reduction from telemedicine | -$80 | -$80 | -$80 | I | |
| Total revenue impact | -$156,800 | -$336,000 | -$672,000 | J | C × H × I |
Facility-related cost savings | |||||
| In-person facility expense per visit | $10.00 | $10.00 | $10.00 | K | |
| Percentage facility cost savings | 0% | 0% | 15% | L | |
| Cost savings per visit | $0 | $0 | $1.50 | M | K × L |
| Total cost savings | $0 | $0 | $63,000 | N | C × M |
Net impact | |||||
| Total net impact | -$183,456 | -$393,120 | -$723,240 | O | E + G + J + N |
| Net impact per visit (overall across all visits) | -$1.31 | -$2.81 | -$6.07 | P | O ÷ A |
| Net impact as a percentage of total department revenue | -0.8% | -1.8% | -3.3% |
*Numbers rounded for illustrative purposes.
This model is intended only to quantify the financial impact of telemedicine as an alternative to in-person visits, with total visit volume remaining the same. It does not consider the impact of utilizing telemedicine to grow incrementally above current visit volumes, which would require additional study.
Other organizations undertaking such a study will almost certainly uncover factors that are unique to their practices and operations that might produce different findings. That said, many of the takeaways from our study are likely to have broad relevance for other organizations and reflect commonalities we share with them (see the sidebar below).
Implications, and a beginning
On the surface, appropriately utilized telemedicine appears to offer an efficient lower-cost alternative to an office visit for appropriate patients. In reality, many factors influence the overall economic picture and impact to the provider’s bottom line.
For our specific situation, based on our assumptions and our current telemedicine use rate, we have experienced a –0.8% impact on our bottom line. If we were to increase our rate of telemedicine usage, the adverse impact would be greater, but there is opportunity to offset some of this impact by reaching a critical mass and thereby obtaining economies of scale and expense savings.
Given that the nation’s health systems are operating on thin margins amid rising payment and cost pressures, the findings of our study underscore the need for thoughtful examination to ensure telemedicine is used and supported effectively and sustainably. Our study represents an important beginning of the research needed to make an economic case for the broader use of telehealth services. The study’s findings can provide an initial basis for further discussion on payment rates for telemedicine services with both commercial and government payers.
Nonetheless, many questions remain to be answered. Not all healthcare organizations’ circumstances for delivering telehealth services match those at Penn Medicine, and additional research is needed to understand the diff erences.
Also, our study was conducted within Penn Medicine’s Department of Orthopaedic Surgery, and there are obviously inherent diff erences among specialties and how they operate that would impact results. Other factors to consider include payer mix, given that not all payers reimburse for facility fees. Moreover, our fi ndings account for the loss of revenue from hospital-based services, but this is not always necessarily a factor.
In the end, the goal should be clear to all: Recognizing the potentially huge benefi ts of telemedicine to patients, providers should continue to deliver these services.
Yet if payment for the services proves insuffi cient to cover the full costs of delivering them, healthcare providers will be challenged to deliver them to the extent they are needed or beneficial, to the detriment of the nation’s healthcare system.
Footnotes
a Note: Our study was not designed to evaluate the efficacy or quality in delivering telehealth to patients, nor was it meant to advocate for or question telehealth’s ability to reach patients in their place of need during a global pandemic, notably in rural or remote areas. Our focus was entirely on the economic factors affecting delivery of such services.
b The enterprise includes about 40 surgeons and 40 advanced practice providers across 13 practice sites, which altogether conduct about 140,000 outpatient office visits annually.
10 takeaways from the Penn Medicine Orthopaedic Surgery telemedicine study
Here are the top 10 takeaways from the study of the economics of telemedicine in the Department of Orthopaedics at Penn Medicine, derived from the authors’ analysis as well as feedback and discussions with the health system’s providers.
1. There is limited opportunity for space savings. Providers typically are physically within our outpatient clinic space when delivering telemedicine services — either because they need to be on-site to also deliver in-person visits, or because of the convenience and staff support available related to any connectivity issues. In this model, organizations have little opportunity to reduce and save on facility expenses, unless telemedicine is utilized at a significant rate.
2. Incremental visits or back-filled replacement visits are key. The economics of a telemedicine visit that replaces an in-person visit (the focus of our analysis) are different from those of a visit that stands on its own unrelated to the in-person schedule. In the pandemic environment, in-person visits were being shifted to telemedicine, with potentially no back-fill or reduction in unused facility space costs. In a post-pandemic world, increasing access and volume through the use of telemedicine above and beyond in-person schedules allows for improved access without additional space and facility expenses.
3. The impact of telemedicine is greater for hospital outpatient department (HOPD) practices. Current parity payment policies do not translate to HOPDs, also called provider-based clinics, for Medicare and certain other payers. For HOPDs, which bill and collect separate professional and technical components, the Medicare parity payment covers only the professional component; no technical/facility fees are currently being paid fortelemedicine visits to HOPD practices (other than a telehealth originating-site fee, which does help offset the difference). For example, as shown in the exhibit below, Medicare pays a Level III office visit about $177 for a HOPD in-person visit and $98 for a HOPD telemedicine visit, a 45% reduction.
Medicare payment comparison: Level III established patient office visit
HOPD | Non-HOPD | |||
| In-Person | Telemedicine | In-person | Telemedicine | |
| Professional (99213) | $71.33 | $71.33 | $97.78 | $97.78 |
| Technical/facility (G0463) | $105.98 | $0.00 | $0.00 | $0.00 |
| Telehealth originating-site fee (Q3014) | $0.00 | $26.65 | $0.00 | $0.00 |
| Total | $177.31 | $97.98 | $97.78 | $97.78 |
Based on MAC/Locality 1250201, Metropolitan Philadelphia
This exhibit shows that the Medicare payment rate for a Level III office visit is about $177 for a hospital outpatient department (HOPD) in-person visit and $98 for a HOPD telemedicine visit, a 45% reduction.
4. Greater impact on procedural/surgical based specialties. For specialties that involve shorter visits and higher patient volumes, and that typically require use of several exam rooms at once, it is more difficult to deliver telemedicine visits at the same rate and pace as in-person visits. Specialties involving evaluation and management (E&M) services with longer visit times are better able to keep pace with in-person dynamics. Lower telemedicine noshow rates may offset some of the lost efficiency.
5. Technology costs vary greatly. The cost of the telemedicine platform was very low on a per-visit basis given Penn Medicine’s size and volume of visits. The cost per visit at smaller hospitals and physician groups would be much higher.
6. Dabbling is inefficient. Developing standardized use cases for visit types/patient types/condition types improves the efficiency of telemedicine from a staff support perspective. Economies of scale, workflow optimizations and protocolized utilization can cut down the staff inefficiencies. Of course, without permanent coverage policies in place, it is difficult to invest the time and effort to optimize telehealth delivery without knowing how it will be covered in the long term.
7. Duplicative visits are a lose-lose. We did not compare the appropriate use of telemedicine wholly in place of an in-person visit versus when a telemedicine visit ended up requiring an in-person visit anyway. We concluded that using telemedicine when a patient’s condition or visit reason indicates the need for an in-person visit is not only additive but also is a disservice to the patient and the provider.
8. Needs for radiology services in person supersede questions of convenience. In orthopaedics, patients require imaging for most assessments as well as postoperative visits. The need for imaging to be performed in person limits the true convenience of telemedicine for many visits, given that patients have to go to a site to receive imaging anyway and often opt to come in person for their visit. This situation may impair an organization’s ability to achieve higher levels of telemedicine use for impacted specialties.
9. Radiology in-house volume may decline. For inperson visits, a patient’s imaging is coordinated to be completed right before their appointment in our co-located or adjacent radiology sites. This approach offers convenience to patients, while providing a source of revenue for the health system. Moreover, any patient receiving a telemedicine visit is more likely to have imaging performed at an external site because the lack of an inperson visit eliminates the convenience of having imaging performed concurrently. This tendency of patients impacts the organization’s radiology volume and revenue and requires coordination of the third-party images into its systems.
10. Different patient populations require different levels of support. Age and socioeconomic status play a role in a patient’s technological savviness. Telemedicine visit use rates and issues must be studied to ensure its use is enhancing access and convenience for all, rather than exacerbating disparities in care or creating new disparities.





