Healthcare revenue cycle is the lifeblood of any hospital or health system.
It comprises all the activities that lead to payment for services provided, from patient registration to verification of benefits to care delivery, claim submission and reimbursement. It also involves communication — with patients, insurance companies, government payers such as Medicare and Medicaid.
As one former HFMA Chair describes it, “Efficient, effective revenue cycle management [is] key to our survival. It also directly impacts our ability to contribute to the health and well-being of our communities.”
Breaking down the components of healthcare revenue cycle
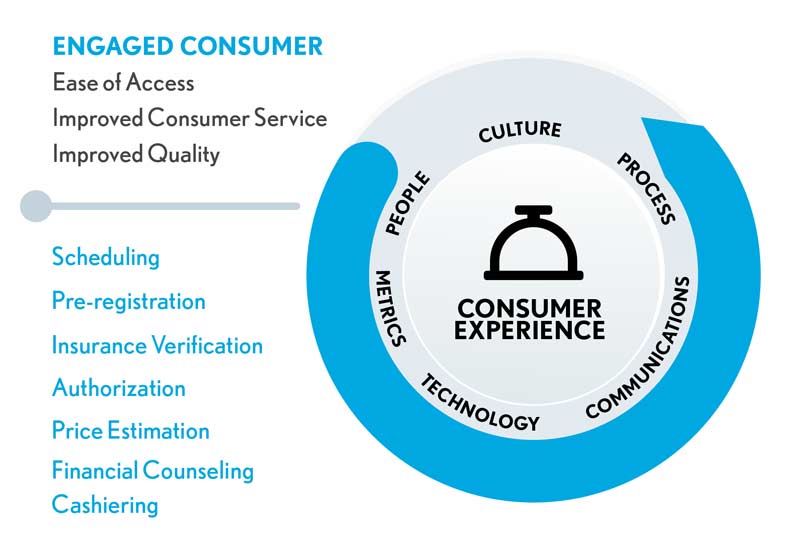
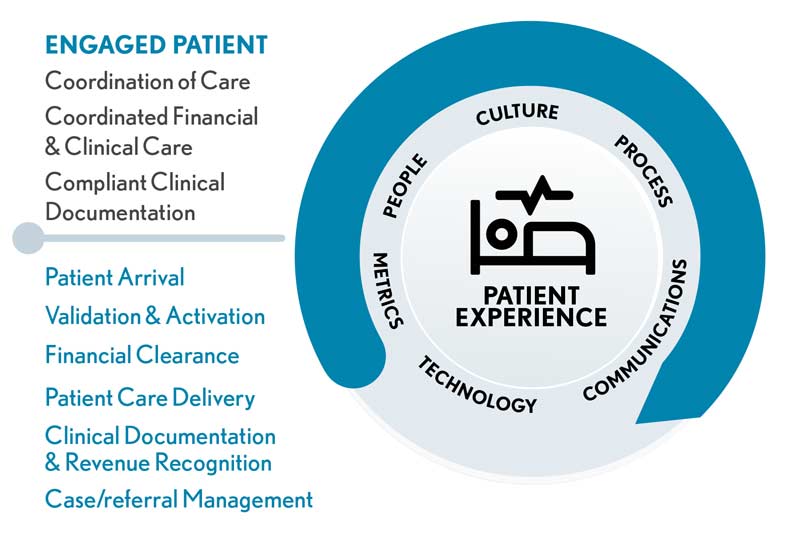
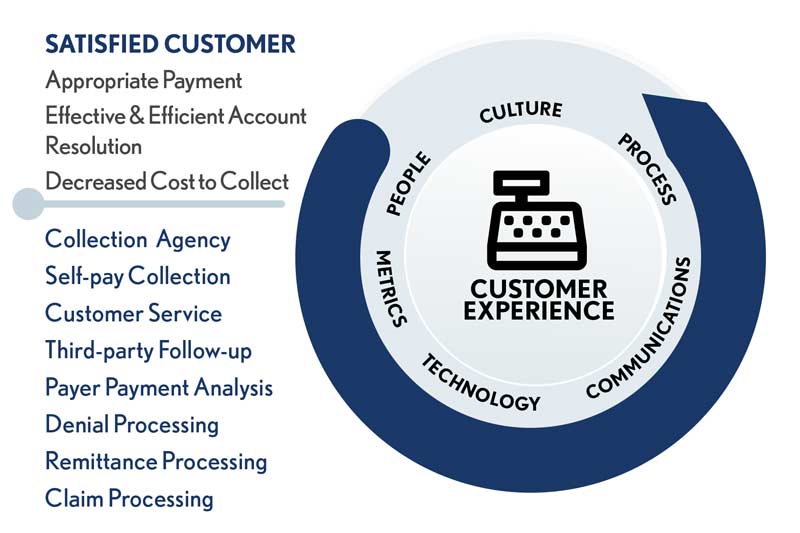
Revenue cycle management depends on more than simply capturing the healthcare services that were delivered and filing a claim for reimbursement. The most effective revenue cycle teams focus on answering the one question patients want to know most: “How much will I pay for my care?” They also look for ways to implement a patient-centric approach to financial communications and engagement. (See the exhibits below.)
Healthcare revenue cycle roles and responsibilities
The patient-centric revenue cyle roadmap
To get there, leading healthcare revenue cycle teams center their efforts on:
-
Price transparency. Now more than ever, people are asking questions about the price of healthcare. Healthcare revenue cycle teams help patients understand the price of the care they will receive, what is included in that price and how much their care will cost after insurance pays its portion. (Find out more in HFMA’s Price Transparency Report.)
-
Supporting equitable access to care. Revenue cycle staff assist patients with applying for financial assistance, when needed. They can also establish payment arrangements that meet patients’ individual needs, according to hospital policy.
Financial conversations with patients. This includes educating patients on the cost of the care they will receive, their insurance coverage and their individual responsibility. It also involves taking the time to understand an individual’s financial situation and determine the best way for the patient to manage their healthcare costs. HFMA has published best practices around:
- When and where financial conversations may be conducted
- Who would be best to participate in these discussions
- What topics should be covered
- Guidance for discussing issues such as financial assistance and prior balances
Find out more in HFMA’s FAQs about Patient Financial Communications.
-
Documentation of care received. In healthcare revenue cycle, charge capture is essential. To process an insurance claim for healthcare services, every aspect of care must be accurately captured. Unless charge capture is performed correctly, the hospital or healthcare facility will not be paid for the care and services provided.
-
Claim processing. Healthcare claim processing is complex work. From scheduling patient appointments to filing a claim with the patient’s insurance company, attention to detail and data integrity — the degree to which data are accurate and complete — are critical. Unless claims are filed in a timely manner, include all of the information necessary to process the claim, and sent to the correct place, the claim could easily be denied. When this happens, a healthcare provider will not receive payment unless it can successfully appeal the denial.
In healthcare revenue cycle, there are specialists who focus solely on claim processing as well as experts in denials management. Find out more about what goes into this process from HFMA’s Claim Integrity Task Force.
-
Medical account resolution. Just as there are best practices for patient financial communications, there are also standards for medical account resolution, such as engaging patients in paying for their healthcare bill. Healthcare revenue cycle teams commit to creating a positive patient financial experience for consumers. This means treating patients with respect while helping them identify sources of coverage, identify opportunities for financial assistance or other discounts; and structuring payment plans that meet the needs of both patients and providers. When hospitals struggle to reach patients to settle their account, medical account resolution specialists work to engage patients in their financial responsibility. These specialists are highly skilled in customer service and have a strong understanding of every aspect of claim processing and reconciliation.
For more information, see HFMA’s Best Practices for Medical Account Resolution.
At every point in healthcare revenue cycle, team members seek ways to provide the best experience for patients, family members and care providers. That’s because the healthcare revenue cycle is critical to the patient experience of care. It’s the first touchpoint patients have with a health system and the last encounter patients will remember. The quality of this experience can determine whether patients return for care or choose another provider.
Looking for more revenue cycle resources? Join HFMA and for one price unlock:
-
Unlimited revenue cycle news stories and online content
-
All live and on-demand webinars
-
All e-learning courses
-
All professional certifications including the Certified Revenue Cycle Representative (CRCR)
-
The online member community including the Revenue Cycle Forum
-
Discounts on live education including HFMA’s Revenue Cycle Conference
-
Local chapter membership
Not ready to join? Sign up for a free 30-day membership trial





