- CMS on Sept. 26 published its discharge planning rule requiring hospitals to provide cost and quality measures on PAC providers so patients can make an informed decision.
- Providing patients and their families with cost and quality data about the post-acute providers available has been shown to reduce costs and improve outcomes.
CMS this week published its long-awaited discharge planning rule. The rule requires that if a patient is being discharged to a post-acute care (PAC) provider, that the hospital’s care team must “assist patients, their families, or the patient’s representative in selecting a PAC provider by sharing key performance data. This includes performance on important quality measures and resource-use measures — including measures related to the number of pressure ulcers in a given facility, the proportion of falls that lead to injury, and the number of readmissions back to the hospital.”
More generally, the rule requires hospitals to focus on the patient’s goals and treatment preferences as part of the discharge planning process. Hospitals are also required to ensure each patient can access their medical record in an electronic format.
HFMA will publish an executive summary of the proposed rule shortly.
Takeaway
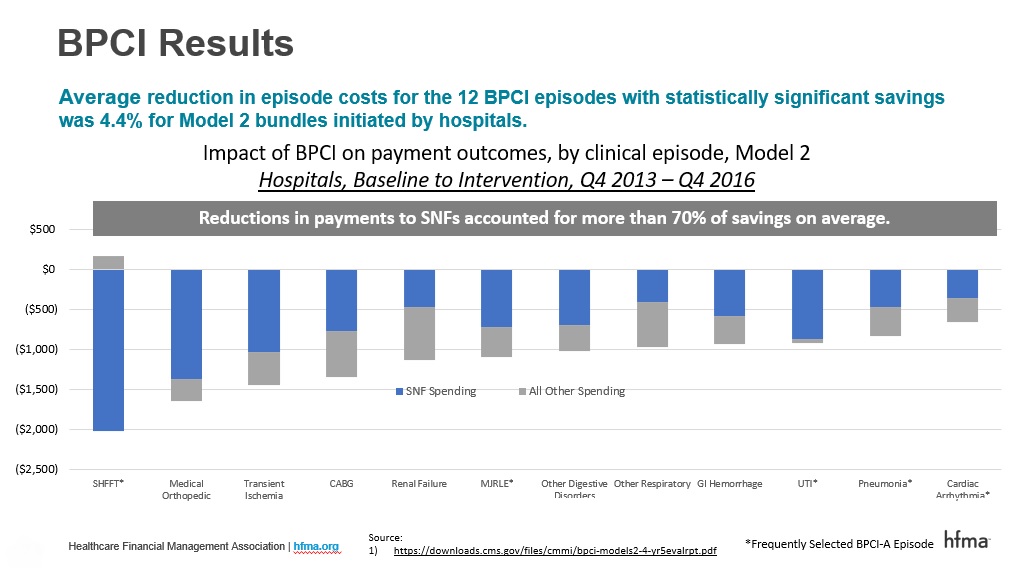
Providing patients and their families with cost and quality data about the post-acute providers available so they can make an informed choice has been shown to reduce costs and improve outcomes. As illustrated by the slide below, the lion’s share of savings from BPCI episodes (BPCI-A’s precursor) came from reduced unnecessary utilization of institutional settings of post-acute care (both by replacing discharges to skilled nursing facilities (SNFs) with discharge to home with home health and by reducing the number of days in a SNF when an institutional stay is needed).
Better practices to educate patients on PAC options
One of the keys to doing this is using cost and quality data to educate patients and their families about their institutional PAC options. HFMA has recently profiled better practices used by organizations participating in alternative payment models to educate patients on their post-acute options:
- Why PAC discharge choices are key to success under risk-based payments
- 3 essentials for creating and managing a high-value PAC Network
Although hospitals participating in alternative payment models like BPCI-Advanced and Next Gen ACO models have long had the ability to provide patients with this type of information to help guide patient decision-making, some organizations have been hesitant to do so due to CMS’s longstanding requirement that providers also not interfere or influence patient choice.
However, this final rule should help clarify that and allow more providers to succeed in these programs in the near term. I anticipate that as hospitals implement this requirement, it will reduce Medicare spending (and benchmarks for episodes of care in BPCI-A and the next iteration of CJR) as Medicare patients choose higher-value PAC providers when they need institutional care.





