7 steps toward compensating primary care physicians for their true value
Even as primary care physicians stand courageously on the frontline in the battle against COVID-19, industry observers are raising concerns that their practice may not be sustainable under the current payment system.
These concerns have risen with the growing awareness of the disparity in compensation between primary care providers and other specialists, which has become increasingly evident amid the COVID-19 crisis. This disparity points out a continuing flaw in the primary care payment structure.
The problem
Although primary care providers are expected to take a wholistic approach toward managing their patient population’s health, they continue to be paid on volume-based formulas. In the past 10 years, CMS has introduced additional payment sources for primary care, including chronic care management, transitional care management and annual wellness visits. These additional sources represent improvements, but they have been implemented within the same flawed reimbursement structure and have therefore not solved the problem.
CMS also offers accountable care organizations (ACO) as another population health vehicle in which primary care physicians play an instrumental role. Yet the ACO model also retains the fee-for-service structure and delays any potential for shared savings for months into the future. Patients would be better served if primary care physicians were paid for the results they are asked to achieve rather than have them continue to be paid through the flawed volume-based model.
The solution
A value-based payment model for primary care would be consistent with the goal of population health, which is to achieve better health outcomes for a population of patients at the lowest possible costs. A key objective for patients with multiple chronic conditions is to reduce the episodes of high acuity, thereby reducing emergency visits and hospital admissions. For the healthier population, the primary care physician team would be expected to manage each patient’s health conditions and activities to promote wellness and prevent a decline in health status.
In each case, the approach to achieving better outcomes is through engagement of the patient in a customized plan of care with the support of the primary care team led by the physician. A more effective primary care payment model would therefore reflect the need for continuous care plan management and reward improved outcomes as well as reduced costs. This model would begin by allocating a percentage of the assigned patients’ per-member-per-month premiums for primary care services. Next, adjustments would made to this allocation based on the composite health status of all assigned patients. The health status adjusted allocation would then be adjusted up or down based on the primary care team’s performance.
How to implement the new approach
The following seven steps offer a pathway for achieving this model.
1. Establish true patient panels for each primary care physician. This step involves instituting formal pairings of patients and primary care physicians.
2. Agree on the optimal percentage of the healthcare dollar that should go for primary care. Currently, 3% to 8% of the healthcare dollar goes to primary care. Given the goal of continuous care plan management, a larger portion of the healthcare dollar should be allocated to primary care to pay for more intensive services. This larger allocation ultimately should reduce total healthcare expenditures by saving significantly more dollars in downstream medical costs. This model should also decrease a significant portion of administrative costs tied up in fee-for-service billing and third-party payer utilization management. Although the optimal percentage allocation to primary care has yet to be defined, it is reasonable to increase the allocation to 10% in this model given the elevated expectations set for the primary care team. The total cost adjustment in step six will move this percentage toward the most appropriate level.
3. Adjust each primary care team’s payments to account for the overall health status of the patient panel. This adjustment is made using the composite patient panel risk adjustment factor (RAF) index based on hierarchical condition category (HCC) rankings.
4. Set targeted performance levels for quality based on primary care scores under the Merit-based incentive payment system (MIPS). The primary care team’s quality performance index can be determined by dividing the team’s actual scores by the targeted performance.
5. Use national primary care patient satisfaction benchmarks to agree on targeted performance levels for service. The primary care team’s service performance index should be determined following the same process used for calculating the quality index.
6. Use current regional healthcare per-member-per-month (PMPM) costs adjusted by the patient-panel-specific RAF score to set a total cost baseline for each primary care team. The cost performance index equals the reciprocal of the team’s actual PMPM costs divided by the baseline.
7. Determine the total value of primary care payments for the period of service. Multiply the quality, service and cost indices by the RAF-adjusted primary care allocations.
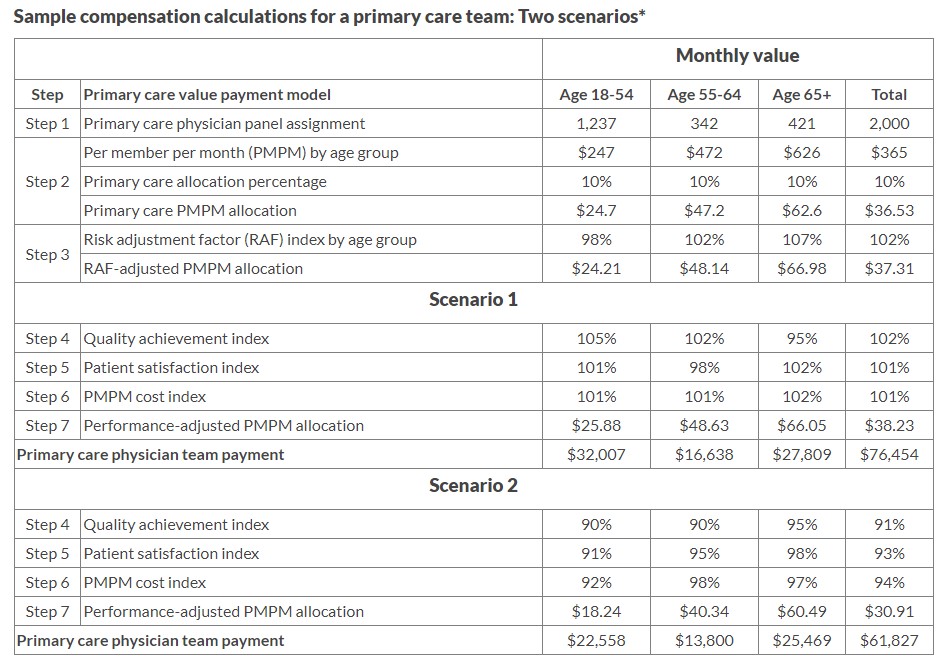
The following table offers two examples of the compensation calculation for two primary care teams with the same sized panels (2,000 patients) and the same RAF scores. The table demonstrates the impact of performance differences on the final primary care payments.
Model benefits
This model is intended to align primary care and third-party payer interests by compensating the primary care teams based on their ability to achieve desired results of population health. The RAF-adjusted primary care allocations remove the team’s focus from delivering care incrementally to managing patient care based on a care plan. The MIPS, patient satisfaction and cost targets identify the desired results for quality, services and total healthcare expenditures, respectively. The indexes generated by comparing actual performance with these targets present a mechanism to pay the primary care team based on their level of achievement. Under this model, the primary care team is empowered to work within its available resources to determine the optimal level of effort required for each patient’s care to achieve the desired results. In a learning environment, the primary care team should assess the results of their decisions each month and adjust their practices to reach a higher level of performance in subsequent periods. This model offers the clear promise of supporting the long-term sustainability of primary care services while increasingly improving outcomes and continuously decreasing costs.





