Focus on care transitions brings substantial new LOS-reduction opportunities
Improving processes to minimize the time patients spend receiving inpatient care continues to be a top hospital priority in today’s evolving healthcare environment.
Reducing the length of stay (LOS) is a well-recognized best place for hospital leaders to transform their organizations’ operations to reduce costs effectively. A focus on redesigning clinical and financial processes to ensure every patient receives the right care, in the right setting, at the right time and with the right workforce is imperative to this initiative’s success.
Because issues contributing to increased LOS commonly arise during care transitions, increased leadership analysis of these points in a patient’s care process can identify significant not-yet-discovered LOS-reduction opportunities. This type of analysis also can uncover opportunities to improve patient experience, satisfaction and safety; promote greater efficiency; and achieve savings from reduced excess patient days in the hospital and better throughput across the continuum of care.
Following are recommendations on where to focus efforts on reducing LOS, and how to derive associated operating and financial benefits, based on lessons learned from LOS-reduction initiatives in hospitals and health systems nationwide.
Review the care management model for improvement opportunities
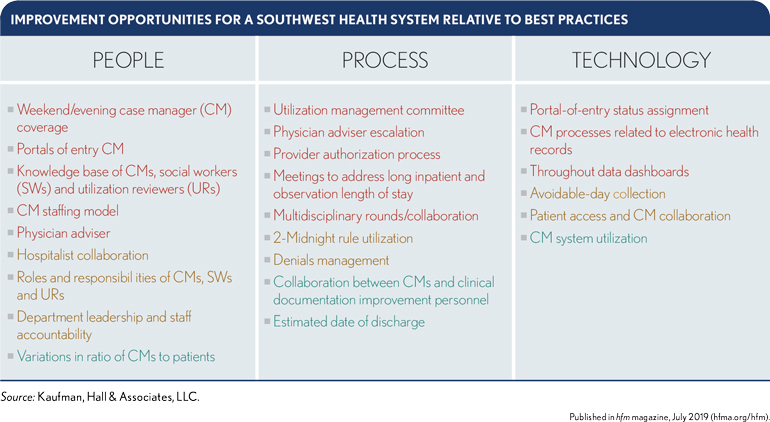
The search for LOS-improvement opportunities should begin with a review of the organization’s care management model, with a focus on the domains of people, processes and technology and their specific roles in coordinating a patient’s care at every step through the care continuum. These domains should form a synergy, working together to ensure the patientcare journey is well coordinated from the entry portal through discharge to the appropriate level of post-acute care.
By comparing their organization’s current performance with best practices identified among all hospitals around the country, a hospital’s leaders can identify promising improvement opportunities in each domain.
The exhibit below illustrates the results of such an analysis for one large hospital in the South, where the items in red indicate areas where the hospital’s practices were furthest from the best practices, thus indicating the greatest opportunity for improvement in the care-management process. For this hospital, the entry portal’s case manager coverage and the portals-of-entry status assignment were among the greatest opportunities for improvement.
Review care transitions during three phases of acute care
A patient’s overall acute care experience involves transitions during three stages:
- Entry into the care system through an entry portal (i.e., the emergency department [ED], surgery, direct admission, transfer or other)
- Experience of acute-care delivery
- Discharge to home or post-acute care
Figure: exit rich text editor to add content
The primary focus of an LOS-reduction initiative should be on improving care transitions during these phases. But the exhibit also shows that attention should be devoted to utilization review and denials management, because these areas can have a bearing on excess patient days in the hospital. The sidebar provides recommendations on improvements to these areas that can help a hospital reduce LOS.
4 recommendations for improving portal-of-entry processes
Based on our experience, four improvements to care transitions at the portals of entry can effectively reduce LOS.
1. Develop a patient flow process encompassing all portals of entry and the role of the command center or bed control. This is a crucial first step of the care-redesign process. To minimize unnecessary acute care days, staff must manage patients appropriately at every portal of entry, ensuring assignment of the right patient status and prompt initiation of discharge planning.
2. Develop a process for multidisciplinary communication that occurs at least every three hours in the ED with a focus on ensuring patientstatus assignments are accurate and discharge interventions are appropriate and timely. It is critical that each patient’s status assignment and readiness for discharge be communicated to and understood by the command center, physicians, nursing staff, case managers and ancillary providers.
3. Thoroughly evaluate and map precertification processes and requirements. The requirements should be documented and clear to all relevant staff, particularly those charged with contacting the insurer to obtain appropriate authorization and precertification for admission and surgery.
4. Collaborate with the finance team to implement necessary process changes. Frequent communication with the central or hospital business office can be an indicator of problem areas, such as insurance denials, that require special attention for process improvements to mitigate the problems.
In sum, such efforts should yield the following results, all of which also will contribute to reduced LOS:
- Seamless patient admission and accurate patient status assignment
- Appropriate management of patients from all portals of entry
- System-wide understanding of precertification requirements and the ramifications of noncompliance
Moreover, by consistently identifying and implementing needed changes for preventing denials, and by identifying and resolving payer eligibility issues and gaps in coverage early, hospital leaders can set the stage for the next phase of the redesign process.
Recommendations for improving acute care and post-acute care processes
Four improvements to care transitions during acute care and post-acute care processes also have been shown to reduce LOS in hospitals.
1. Establish meetings to discuss patients at risk for an extended stay either in inpatient care or outpatient observation. These meetings should be attended by the physician adviser, hospitalist leadership, utilization managers, case managers, social workers, ancillary staff, nursing staff and business office/revenue cycle leadership. The goal of these meetings should be to ensure each patient’s timely progress through the inpatient stay, with an appropriate, well-timed discharge plan in place and ready to be executed.
2. Implement multidisciplinary rounds (MDRs), with a focus on interdisciplinary collaboration, for all patients on all units. Having the entire team participate in daily MDRs not only improves collaboration among disciplines, but also results in increased patient throughput and earlier discharge times. Such collaboration helps maintain optimal patient flow through the ED and surgical units and achieves the goal of placing the right patient in the right location at the right time. Many organizations include only nursing and physicians in rounds, but a truly multidisciplinary team meeting for a few minutes each day for each patient, with a set agenda and staff scripts, is much more effective.
3. Ensure consistent application of all criteria for patients’ continued stay, focusing on medical necessity and discharge-planning criteria. Staff should receive guidance to consistently apply evidence-based criteria correctly on admission and throughout the continued stay.
4. Track, trend, report and act on avoidable days to improve processes. Patient admissions on a Friday, for example, are one of the more common reasons for avoidable days and/or delays when there is a lack of available testing or ancillary services at the facility on the weekend. Bottlenecks also may occur when discharge times coincide with admissions times, as shown in the exhibit below, which reflects one hospital’s actual experience. Care managers can minimize such bottlenecks through collaborating with post-acute care sites. For example, nursing homes can be encouraged to admit patients earlier in the day (at 10 a.m.) rather than after 2:00 p.m.
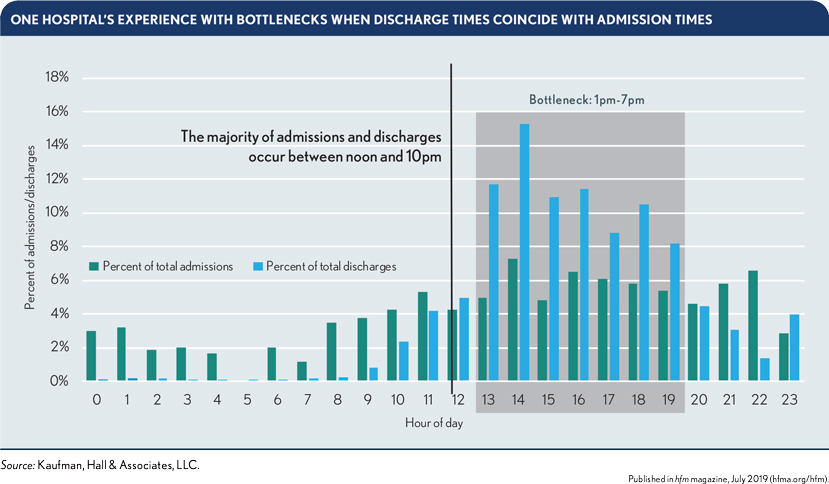
An inclusive family-centered approach, in which discharge plans are developed with the patient’s family, also can help reduce avoidable days. For example, a family member can plan to pick up the patient at a specific, agreed-upon time earlier in the day.
Such efforts in improving acute care and postacute care transition also can result in improved safety and patient satisfaction and better alignment of the organization’s average LOS to the Medicare geometric mean LOS (GMLOS). Using tools that track and trend productivity, a hospital can identify and resolve throughput barriers prior to the anticipated date of patient discharge, thereby advancing toward best-practice performance in care-management processes.
How reduced LOS could improve revenue and cost performance
LOS reductions from improvement-in-care transitions have the potential of producing impressive results. The exhibit below highlights the benefits one organization estimated it could achieve with low (25%), medium (40%) or high (55%) targets for percentage improvement.
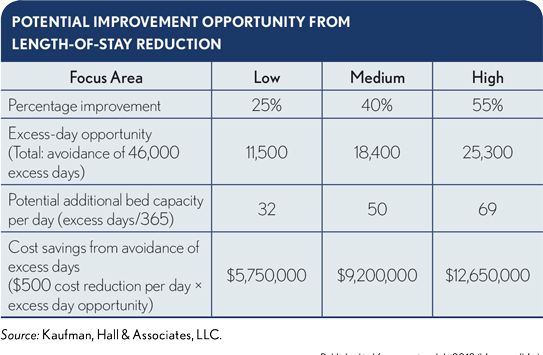
The “excess-day opportunity” of 46,000 days shown in this exhibit is calculated by subtracting the number of inpatient days an organization expected in a fiscal year based on the Medicare GMLOS (in this case, 80,000 expected days) from the observed or actual number of inpatient days (126,000 days) in that same fiscal year.
The numbers in the exhibit represent significant cost reduction of $5.75 million to $12.65 million and revenue-improvement potential of 32 to 69 additional bed capacity, even at the lower end of achieved improvement. Organizations with best practices in care management, using targeted and facility-specific interventions, should be able to reduce excess days, thereby achieving the higher cost savings.





