Healthcare leaders can successfully implement change only to the extent that they address its impact on employees.
The healthcare industry has seen almost constant change since the turn of the century. And the trend shows no sign of stopping soon, driven by technology and the continuous evolution of social and political values. The momentous shift from fee-for-service to outcomes-based payment constitutes one of the greatest challenges the industry has faced, requiring healthcare leaders to become adept at change management to ensure the survival of their organizations. Although there is just one societal end goal, the strategies for addressing this shift will be different for every organization, and each organization must respond and adapt to these pressures uniquely.
But managing change is challenging and requires careful planning and execution. Studies have shown that projects and initiatives across health care and other industries fail more often than they succeed, particularly in IT. a
The Chinese word for change is made from two symbols—one meaning threat, the other meaning opportunity. Healthcare organizations must look for ways to minimize the former and maximize the latter to drive change forward.
Organizational Culture
One such threat to change is longstanding organizational culture. Results of a growing body of social and psychological research suggest that true change must overcome cultural inertia to the point of changing the very culture itself. As former healthcare executive Fred Lee points out in his book If Disney Ran Your Hospital, “Culture trumps strategy, but structures can trump culture.” b
The point is that structural change can, over time, bring about cultural change. Regulators and insurance companies often force change by changing the structure—particularly the structure of payments. Organizationally, however, the response to change imposed from without is different from the response to change imposed from within.
When leaders appear to dictatorially impose too much, staff can push back severely with lagging morale, reduced engagement, varying levels of internal sabotage, and at the extreme, unionization and strikes. Change led internally must be accomplished in ways that are fundamentally different from externally imposed change.
The Stages of Change
People tend to respond to change in four stages, in a manner that can be likened to the grieving process: denial, resistance, exploration, and commitment, as shown in the exhibit below. c
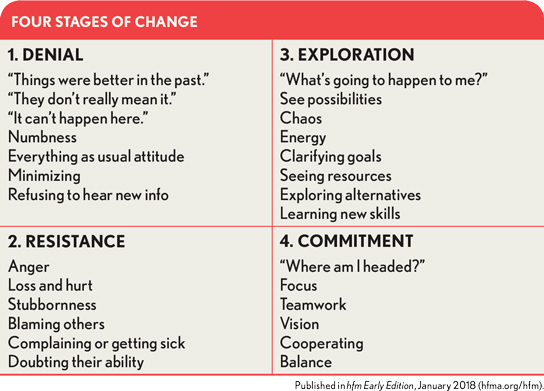
Within the organization, if too many people remain in denial or resistance, the change process will fail. The goal of leadership is to help the majority of the staff choose to accept the change and to move through these first two stages and into the third and fourth stages.
For a change effort to succeed within an organization, leaders must address the intellectual and emotional impact of the change and how process must be altered to accommodate it.
Intellectual impact. To address change from an intellectual standpoint, leaders should consider the logical reason that change is needed and seek to clearly describe the future state and the steps required by everyone to achieve it. Leaders may take the opportunity to provide data showing how others in similar situations successfully adopted the same or similar change. Addressing the factual reasons for change provides a rationale that enables staff to begin visualizing how they could succeed in the new environment.
Emotional impact. Feelings may lead people to move in a new direction without any conscious decision to do so. The power of the emotional engine, believed by many to play the strongest role in solidifying change, is greatest when its effects are subliminal and appeal to positive feelings, because people tend to be most resistant to change if they feel they are being manipulated. Some typical appeals to emotion can revolve around fear, guilt, shame, peace of mind, sense of fair play, pride, and desire to be on the “inside” or part of something truly significant that transcends self-interest. The most rapid, but least permanent, kind of change is that imposed by appeals to fear (e.g., threats of firing employees who do not follow instructions), while positive appeals that connect with a person’s aspirations are the most powerful agents over the long term. Change is most effective when people choose to accept the change because it aligns with some internal need or value that they have.
In American society, we commonly use money to foster acceptance of change, but studies show that, over time, people who do not accept change are the most likely individuals to regard it as onerous, prompting them to make escalating demands for more money. d
Ironically, the utility value of money decreases as the recipient becomes wealthier, leading to reduced value of incentive for the same dollar of expenditure.
Early models of human decision making placed the intellectual process as the starting point to change, leading to a decision that would produce feelings that would then be addressed and resolved. In many instances, however, the initial input into decision making could be the emotional component, leading to subsequent intellectual processes where people seek an intellectual reason to support the change and finally announce their acceptance of it. By recognizing this pattern, we can now devise more effective ways to lead change—for example, by presenting the change incrementally or in a series of small, workable steps.
Social and ethical values—essentially dealing with how we want others to perceive us—can be stronger motivators than financial incentives. If we can link the desired change to being a “good nurse,” for example, all nurses who want to be perceived as good nurses will be inclined to accept the change. Ethical values deal with how people think about themselves. When a change is accepted in terms of an internalized value, the individual’s willingness to embrace the change is dramatically increased. For example, physicians who are frustrated by the increasing paperwork burden imposed by value initiatives may be comforted by the idea that the new processes may lead to better patient care, thereby making them more receptive to embracing the change.
Process change. An effective way to make a desired change easier for staff to absorb, and the status quo more difficult to sustain, is to restructure of the environment through changes in process. For example, one hospital was seeing growing expenses for overnight shipping. Upon reviewing usage of the service, the CFO found that many items did not actually require overnight shipping. In response, he sent an email advising employees that mailers for next-day service would now be kept at his assistant’s desk instead of a self-service box in the mailroom. In subsequent weeks, mailer usage dropped 50 percent.
Another example is offered in the book Switch: How to Change Things When Change is Hard by Chip and Dan Heath. e When banks learned that people were forgetting to remove their debit cards from ATMs after a cash withdrawal, they changed the sequence of events in the software to require that customers remove their cards before cash is dispensed.
Restructuring the environment requires the creation of a new path. In some instances, an organization might build several new paths, finding that some are more effective than others. For example, a health system might take a trial-and-error approach using isolated populations (such as a different path for the same process at a different hospital) or using the same population but presenting the paths in a sequential manger with sufficient time to evaluate the efficacy.
The greatest risk, however, is in creating the wrong path. Consider, for example, how a hospital might implement staffing controls. One possible path a hospital might use is to require any department that is not achieving at least 90 percent on its biweekly productivity report to appeal to a wage committee to fill vacant positions, while permitting departments that are achieving more than 90 percent of biweekly productivity to fill vacant positions simply by completing a requisition form. This solution is problematic in that it ignores an important goal of effective change management, which is to get employees to internalize the desired change. The imposed rule could enforce the desired behavior, but it also could lead managers to use workarounds—such as overtime or reductions in service levels—to bypass the system, rendering it ineffective. Instead of trying to force managers to adhere to an imposed structure, leadership should focus on finding a way to get line managers to make efficient staffing decisions without having to micromanage through a wage committee.
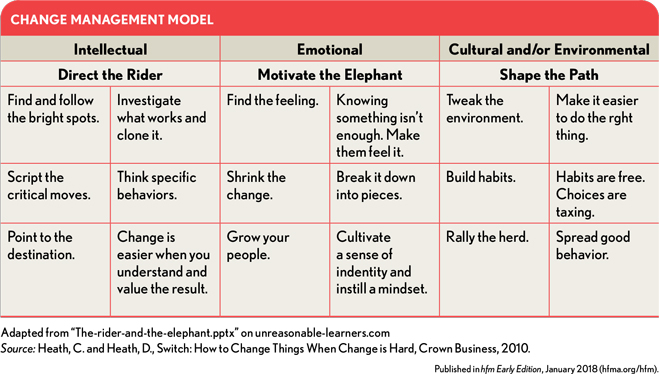
One excellent template for planning change is provided in the Heath brothers’ book. This template is adapted in the exhibit above. Addressing only one or two of these items more effectively might have the benefit of doubling or tripling the rate of adoption of the proposed change.
As the nation’s healthcare system continues to undergo change that is in many ways unprecedented, healthcare leaders require the skills to manage that change in a way that avoids collateral damage to employee engagement. Only through the application of such skills can leaders lead change quickly and effectively, and thereby build a fully market-responsive and successful organization. The principles described are the foundation on which healthcare leaders can begin to build this all-important competency.
Paul Selivanoff, CPA, is principal and lead consultant for Simply Better Outcomes, Lincoln, Neb.
Footnotes
a. “IT Project Failure Rates: Facts and Reasons,” Faeth Coaching.
b. Lee, F., If Disney Ran Your Hospital: 9 ½ Things You Would Do Differently, Second River Healthcare, 2004.
c. Portier, C., “Change Curve: 4 Stages of Change Management Acceptance,” Paragon, May 25, 2016.
d. “Five Things Physicians Need to Stop Doing if They Want to Lead,” WantHealthcare, July 2, 2014.
e. Heath, C. and Heath, D., Switch: How to Change Things When Change is Hard, Crown Business, 2010.





