How smaller organizations use patient experience best practices to improve competitive edge
- Healthcare leaders are recognizing that the revenue cycle is not just about revenue but also about patient engagement.
- Appealing to patients as consumers can put a smaller hospital on a level playing field with larger health systems.
- Convenience and communication are two key strategies for capturing patient loyalty.
At UConn Health, the chief revenue cycle officer decided to experience a typical patient journey. By following patients a few days and months after their care, she identified two opportunities at this academic medical center in central Connecticut.
- Use of video monitors throughout the facility to capture and highlight excellence in clinical areas as well as in patient financial experiences.
- Engaging patients about what to expect after care — the billing process in addition to medical information. UConn Health offers patients the opportunity to discuss the billing process and payment options, which promotes a positive patient response.
It’s this type of attention to patient experience that can offer smaller healthcare organizations and health systems a competitive advantage over larger providers in the area. Ultimately, revenue cycle leaders like those at UConn Health recognize that the revenue cycle is not just about revenue but also about patient engagement. Finding ways to appeal to patients as consumers can put a smaller hospital on a level playing field with larger health systems.
At every point in the patient journey, besides care delivery, revenue cycle has an opportunity to enhance patient experience. Faced with competition from large healthcare organizations, many small health systems offer financial payment options to ensure patients seek care when needed. As part of the process, trained professionals are available for financial conversations at all points in the journey.
Successful strategies to improve competitive advantage can be framed in five Cs — convenience, culture, communication, C-suite leadership and commitment.
Convenience. We find that convenience takes on two forms. First, consider the convenience of accessing care. Smaller providers must initially focus on price-competitive service lines that best fit community needs. Once they determined the services they can provide at competitive prices, smaller providers can create partnership strategies for the service lines they don’t offer. Those may include telemedicine or video consultations with specialists or referral arrangements with other local healthcare providers.
The second form is convenience in the patient-care experience. Leverage technology to ensure the entire patient experience is as painless as possible — scheduling, getting price estimates, providing care, and understanding and paying bills.
Culture. Though culture can have many contexts, the importance of patient engagement in value-based care requires that healthcare organizations look at healthcare delivery from a patient’s perspective. For example, Mosaic Life Care in St. Joseph, Missouri, focuses on patient experience, including awareness of language used in patient interactions. Healthcare jargon such as “episode” or “encounter” has been removed in favor of more common language. Talking with patients in everyday language promotes a more personalized, small-town service from smaller providers.
Communication. As revenue cycle teams develop strategies to boost competition, it is important to improve estimation processes and proactively discuss payment options, ideally before services take place. The key is to balance strong communication with accounts receivable (A/R) goals. To meet that strategy, one Minnesota health system invested in training financial counselors and worked with the marketing department to ensure financial policies, payment options and payment methods are consistently communicated across all points of patient engagement. This approach tends to generate more questions during the registration process, but it results in more informed patients and an increase in patient payments — up front and on the back end.
C-suite leadership. Though similar to culture, C-suite leadership is focused on ensuring organizational leaders support revenue cycle teams. In smaller communities, it is critical that C-suite leaders connect with other community leaders to ensure transparency and foster a sense of local ownership for the long-term financial health of their health system.
For example, MaineGeneral Health often saw its patients drive south to Boston for care. Revenue cycle leaders recognized they needed to find ways to keep patients closer to home. A key tactic was revamping its patient financing options through a third-party vendor. When the system switched from managing long-term payment plans internally to outsourcing, the change also affected employee payment options. Recognizing employees are just as important a patient constituent group as non-employees, the CEO advocated to communicate the change and assure employees throughout the transition.
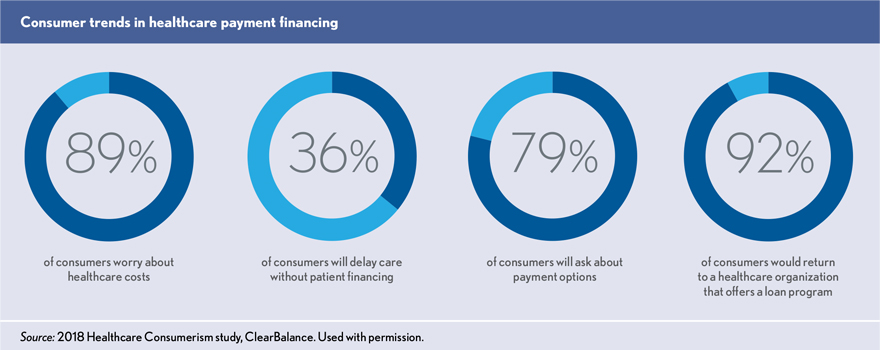
Commitment. Patient loyalty depends heavily on earning their commitment to support and return to your health system. By engaging in proven, proactive strategies, it’s possible to secure commitment from patients. Health system leaders find that offering zero-interest patient financing has been a key driver for loyalty and word-of-mouth referral. According to ClearBalance’s 2018 Healthcare Consumerism study, 92% of patients very likely will return to a health system because of the availability of long-term patient financing, and 89% will refer family and friends. Knowing that they have a way to affordably manage their out-of-pocket medical costs, patients can focus on the care experience.
Finally, health systems should align with their patient experience and financial goals. Smaller community providers don’t have to spend their way to a better patient experience. By focusing on the five Cs and ensuring their strategies put the patient first, these providers can provide patient experiences that promote loyalty, deliver optimal payment and offer a leg up to compete with larger health systems.
Learn from best-in-class organizations and industry thought leaders about the latest revenue cycle practices. Save the date for HFMA’s Revenue Cycle Conference, March 30–April 1, 2020, in New Orleans.





