Creative partnerships bring relief from soaring drug prices
A large health system and a multispecialty clinic have gotten a handle on drug costs through close collaborations with outside entities.
- The lack of affordability of many prescription drugs is affecting the patient experience and healthcare outcomes.
- Regardless of whether policy solutions emerge from Congress or the White House, providers are taking the initiative to tackle the problem.
- One of the nation’s largest health systems worked with a vendor to establish a specialty pharmacy, improving access to vital drugs and reducing costs.
- A multispecialty clinic and regional health plan collaborated on a mechanism that nudges physicians to prescribe less-expensive drugs.
After receiving a diagnosis of hepatitis C, Yvonne Nicholson learned about her treatment options. A drug called Harvoni, which has emerged as a leading choice of prescribing physicians since the FDA approved it in October 2014, could cure the disease if taken for a 12-week period.
The obvious concern was the price tag: $1,000 per pill and $81,000 for the full regimen.
Given that Medicare covered only part of the cost, Nicholson could not have afforded the medication without help from the specialty pharmacy program at St. Joseph’s Hospital & Medical Center in Phoenix. Staff at the specialty pharmacy arranged for a charitable grant to cover the balance, ensuring Nicholson would pay nothing out of pocket.
Nicholson was impressed with the service she received from the pharmacy, the product of a partnership between St. Joseph’s parent company, Dignity Health, and a specialty pharmacy integrator. In addition to securing financial assistance, the pharmacy helped with procuring the medicine, managing delivery and following up on care.
“The pharmacy made the medication totally accessible,” says Nicholson, 72. “Once I told them I couldn’t afford the medication, they said, ‘Don’t worry about it. We’ll let you know within 48 hours if we have a grant for you.’”
The cost of the medication illustrates the scope of the drug affordability barrier that patients confront every day, while the specialty pharmacy exemplifies the efforts initiated by hospitals and health systems to find solutions.
Skyrocketing prices lead to a search for answers
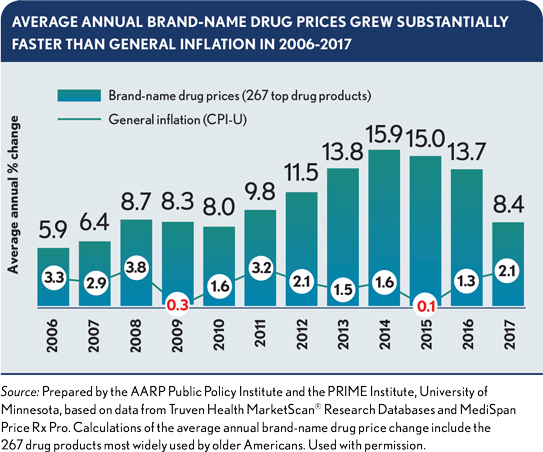
From 2006 to 2017, the average annual retail price of a brand-name drug in the United States increased by 264%, from $1,868 to $6,798. Prices climbed at double-digit rates annually from 2012 to 2016, peaking with a 15.9% spike in 2014.a A large part of the cost escalation has been due to specialty drugs, which are used to treat complex, chronic or rare conditions. Per capita spending on those drugs increased by 48% from 2013 to 2016.b
Given such trends, drug costs have become a central focus of healthcare policy. Democrats in Congress have proposed various legislative solutions, such as authorizing the Department of Health and Human Services to negotiate lower prices for drugs under Medicare Part D. The Trump Administration in 2018 released a blueprint to address the issue, emphasizing transparency and simplification through regulatory steps.

Some hospitals and health systems don’t want to wait to for policy approaches to take effect, even as they recognize the need for bold solutions. They are partnering with other healthcare stakeholders in initiatives to improve the cost and accessibility of drugs for their patients.
“Pharmacy spend is a huge issue,” says Peggy Sanborn, corporate senior vice president of partnerships and joint ventures for CommonSpirit Health, which was formed by the 2019 merger of Dignity Health and Catholic Health Initiatives.
“As the number of costly specialty drugs available to patients increased, we knew we needed to look outside of our system for a new way to help those with chronic conditions,” she says. “We found a partner not only with expertise in the specialty pharmacy market, but one that is also aligned with our mission to provide the highest-quality of care to all — in this case, to patients who are often facing one of the most challenging times in their lives.”
Launching a specialty pharmacy to improve drug access
In collaboration with its vendor partner, Dignity Health, a not-for-profit network of 41 acute care hospitals in Arizona, California and Nevada, launched the specialty pharmacy program in its Phoenix and Sacramento markets in the summer of 2018. The pharmacy provides medication for more than 20 disease states, including arthritis, cancer, cystic fibrosis and multiple sclerosis.
The vendor procures and processes the medications through a centralized function. Dignity licenses the pharmacies and employs the pharmacists.
The vendor also has 14 pharmacy liaisons who work on-site at 35 Dignity-owned clinics to help physicians and patients with medication acquisition and adherence and with finding resources that can assist with out-of-pocket costs.
The impact: Before the specialty pharmacy program was launched, the process for getting patients on their prescribed medications could take as long as several weeks, financial-assistance support was inconsistent and patients and physicians faced more of a burden in getting medication approved.
In its first 10 months, the program:
- Served 1,500 unique patients
- Processed 1,800 prior authorizations
- Fulfilled 4,800 prescriptions
The program also has generated $8.3 million in patient financial assistance and about $125,000 in cost avoidance for patients across 900 clinical engagements and 75 clinical interventions.
“We’ve been able to significantly shorten the time from the doctor selecting a pharmaceutical protocol on a specialty drug and getting the patient on the drug, in some cases in just a couple of days versus a couple of weeks,” Sanborn says.
The specialty pharmacy certainly worked for Nicholson. She completed her medication in 12 weeks, no longer has hepatitis C and is in good health. “It’s such a blessing and such a gift. I never expected to be able to take that medication,” she says. “Thanks for that pharmacy.”
Dignity Health has expanded the pharmacy program to the Los Angeles market and expects to implement it in the Northern California, Bakersfield and Nevada markets by the end of the year.
Making it easier to prescribe affordable generic drugs
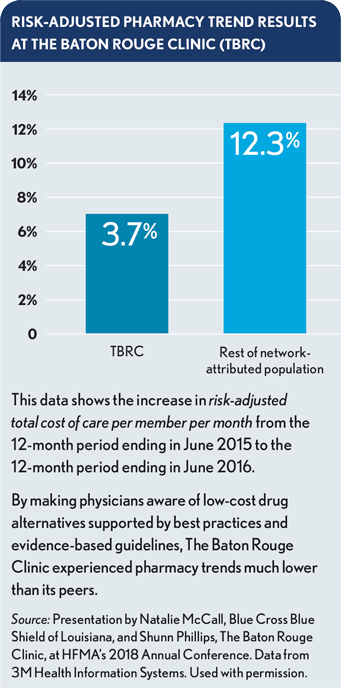
In conjunction with a shared-savings program initiated in 2014 with its health plan partner, The Baton Rouge Clinic (TBRC) began prescribing more generic medications in a quest to curb pharmacy costs. Using data supplied by its partner, Blue Cross and Blue Shield of Louisiana, TBRC created hard stops in its electronic health record to alert physicians about lower-cost alternatives to high-cost drugs.
A team from Blue Cross, including a data analyst, population health pharmacist and medical director, examined claims data to identify high-cost drugs used by the TBRC-attributed population in the health plan’s accountable care organization (ACO). The Blue Cross clinical team then recommended clinically effective, lower-cost alternatives and reviewed them with TBRC physician leaders.
A key driver of savings was the Blue Cross pharmacist’s recommendation to use generic alternatives rather than generic equivalents, says Natalie McCall, director of accountable care engagement for Blue Cross Blue and Shield of Louisiana. Unlike equivalents, alternative medications do not have the same active ingredients as their brand-name counterparts. But in many cases, they are effective in treating the same condition while costing much less, McCall says.
For example, the pharmacist recommended an alternative medication to treat high cholesterol rather than the brand name or its generic equivalent. Per prescription, the difference in cost was hundreds of dollars relative to the brand name and tens of dollars relative to the generic equivalent, McCall says. “I think that was something very unique about what she did,” McCall says.
Shunn Phillips, CFO and compliance officer for TBRC, says physicians generally were very receptive to using less-expensive alternatives, especially given the prospect of improving medication adherence by offering more-affordable options to patients.
However, there was some pushback. Physicians resisted switching to a less-expensive medication when a patient was not complying with the brand name — or when a patient, especially an elderly patient, had been using the medication for a long time.
Consequently, the program has been more successful with new prescriptions, which Phillips attributes in large part to the electronic alerts. “Anytime you can give information to a physician at the point of action, it’s always so much more helpful,” Phillips says.
The impact: The use of lower-cost alternative medications is affecting pharmacy costs and medication adherence for TBRC patients. From 2017 to 2018, the increase in pharmacy spend for the TBRC-attributed population (on a non-risk-adjusted basis) was 60% lower than for attributed patients in all Blue Cross ACOs, McCall says.
McCall says TBRC also is a top performer in the health plan’s Quality Blue Primary Care Outcomes program, which gauges how well providers manage chronic conditions. At TBRC, for example, 87% of patients with hypertension have the condition under control, defined as a blood pressure reading of less than 140/90.
“Baton Rouge Clinic is keeping patients adherent in part through more cost-effective medication,” McCall says.
“We feel like we are having a positive impact on patient outcomes,” Phillips says. “When patients can afford their treatment regimen, they’re more likely to stick to it.”
Footnotes
a. Schondelmeyer, S.W., and Purvis, L., “Brand Name Prescription Drug Prices Increase Four Times Faster than Inflation in 2017,” AARP Public Policy Institute, September 2018.
b. “Medicine Use and Spending in the U.S.,” IQVIA, May 9, 2019.
Tips for effective partnering

A provider leader and health plan leader offer these tips for succeeding in a joint venture to bring down healthcare costs:
Initiate the dialogue
Providers should engage health plans and ask questions, be willing to discuss options for ways to partner, and find common goals and work together to achieve them. The sides should have regular conversations about where they are seeing spikes in the cost of care.
Start small
Providers should be willing to try pilot projects that involve small groups of participants so that potential issues can be identified and corrected before rolling out the plan on a larger scale.
Validate and use data
Providers should take advantage of their health plan partner’s access to claims information. It is important to confirm the accuracy of the data before sharing it with physicians for use in patient care.

Be transparent
In its joint venture with The Baton Rouge Clinic (TBRC), Blue Cross supplied physicians with information about the cost of brand-name medications and about the impact of reducing overall pharmacy spend on costs and medication adherence.
Ensure data is accurate
Blue Cross analysts, rather than external agencies, were the source of the data on existing brand-name medications and lower-cost, generic alternative medications. That meant Blue Cross could more easily address physician questions and ensure accuracy.
Use a dedicated team
Blue Cross supplied TBRC with a team that was dedicated to the accountable care organization and not involved in fee-for-service contracts, enabling the partners to focus on programs that achieve value.





