Front-line stories: How today’s prior authorization processes create a burden of waste for providers

Alan S. Kaplan, MD, MMM, FACPE

Abigail Abongwa, CRCR
The experiences of one health system in contending with administrative waste due to overly complex prior authorization processes demonstrate why addressing this issue should be a prioritiy for our nation’s healthcare system.
U.S. hospitals have been considered recession-proof for decades. Even during the recent Great Recession, the healthcare sector thrived while other economic sectors struggled. The COVID-19 pandemic is different. The scale of job loss is profound, likely leading to a large shift of people from employer-based private insurance to Medicaid. The New England Journal of Medicine estimates that hospitals will lose $95 billion in annual revenue due to the shift from private to public insurance. The American Hospital Association projected that losses for U.S hospitals and systems would amount to at least $323 billion for 2020. The financial footing of U.S hospitals is in jeopardy.
If there was ever a time for healthcare organizations to leave “nothing off the table” in addressing economic challenges, it should be now, during the pandemic. Hospital leaders who are already struggling with razor-thin margins are anxious to tackle activities that, far from adding value for patients, actually impose greater financial burdens. And most would probably place administrative waste high on the list.
In January 2020, when COVID-19 was a minor blip on the radar of healthcare experts, the Annals of Internal Medicine published a major research study that put new numbers to what we already knew to be true: Administrative and regulatory burdens placed upon U.S healthcare providers were ballooning out of control with severe financial consequences.
The study found administration of U.S. healthcare cost $812 billion in 2017. Americans pay over four times more than Canadians for administrative costs. This difference is attributed largely to excessive overhead associated with billing private insurers and private payer involvement in Medicare and Medicaid programs. In total, more than one-third of all healthcare costs in the U.S. were due to insurance company overhead and time providers spend on billing processes.
Impact at the front lines
The national numbers that put a dollar amount on administrative and regulatory waste are staggering. But what occurs at the front lines of care shines an even brighter light on what patients tolerate to obtain care and what patient financial clearance staff endure as they try to advocate for patients and be good stewards of hospital resources. The inefficiency, strain and risk that prior authorization procedures impose on providers and patients offer a case study in how to not manage healthcare administration and regulation.
At a time when payers, providers and patients should be collectively trying to ease barriers to care and push for greater efficiencies, we are instead seeing prior authorization practices morph into such an extreme level of complexity and bureaucracy that multiple industry segments, such as software products, consultants and staffing agencies, have emerged and are thriving as providers struggle to manage processes on their own.
Stories from the front lines
There are countless real-life stories highlighting the inefficiencies and blatant administrative waste that plague the prior authorization process – from incorrect information on insurance websites to uninformed payer staff and an ever-changing set of barriers imposed by insurance companies that burden providers with mounting workloads. Here are just a few.
Incorrect information provided by payers. In early 2019, a brain surgery patient at UW Health came close to having their surgery cancelled because the surgery was approved using benefits for out-of-network providers. A representative for the insurer had incorrectly informed the patient that no in-network providers were available to perform the needed surgery. The patient saved over $200,000 by disputing the insurer’s handling of the claim.
Another UW Health patient was incorrectly listed within a major commercial payer’s system as having both Medicare Parts A and B as their primary insurance, thus making the commercial coverage secondary. However, when verifying this information, the UW Health financial clearance representative discovered the patient had only Medicare Part A. Because the patient’s surgery was to be performed on an outpatient basis, the secondary commercial coverage should become primary. UW Health spoke to four representatives from the commercial payer trying to resolve this issue and initiate the authorization. The payer would not allow the prior authorization to be submitted and instead asked that UW Health deliver the service, submit the claim and then wait to see if the payer would pay for it.
Because the payer had clearly stated that prior authorization was required for this outpatient surgery, UW Health would not agree to moving ahead with the surgery, because payment would likely be denied. The UW Health financial clearance staff spent many more hours on the phone trying to resolve this case unsuccessfully. The aftermath included three hours of un-utilized OR time and a very frustrated patient and clinical team. The case was restarted from scratch, with surgery scheduled four months after the original surgery date due to the insurer’s incorrect database and inability to correct its own data issues.
The life of a typical pre-authorization request for surgery
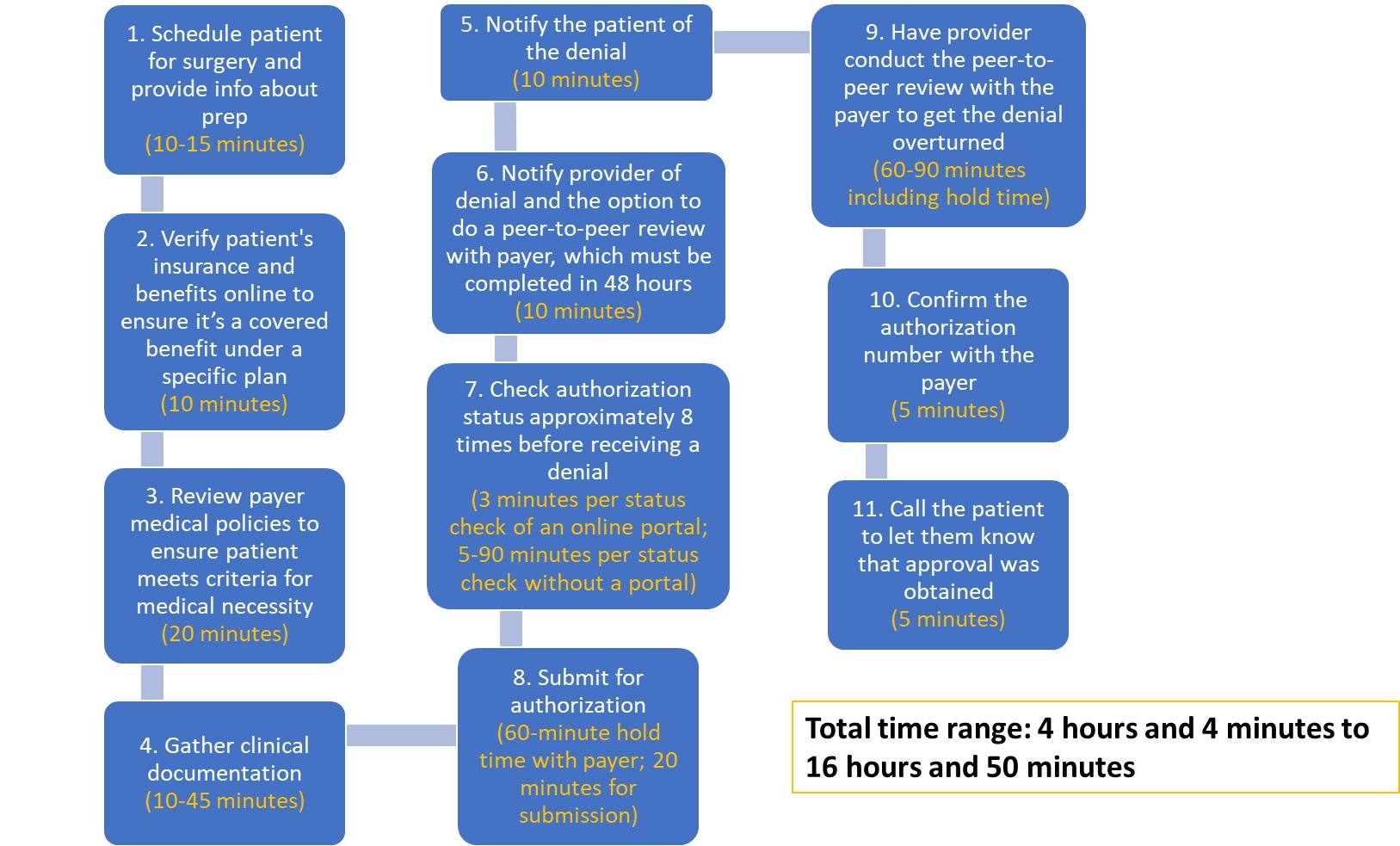
Source: UW health, 2021
Each step has nuances and variations in time required, depending upon the payer and the procedure. Phone calls are often used to verify information located online to provide back-up documentation. In worst-case scenarios, payer websites may be down. In addition, if an inpatient stay is required, that is a separate authorization process.
An out-of-network plan refusing to pay anything for a patient with out-of-network benefits. Many payers now require both a referral from the patient’s primary care physician and prior authorization before they will approve coverage of care out of network, which can take two weeks or longer to process. In one case at UW Health, the insurance plan for a large manufacturer threatened to refuse any payment for a procedure for one of its employees unless an out-of-network referral was sent electronically by the primary care provider. This major insurer refused to pay anything for out-of-network care, even though the patient’s benefits would have covered care at an in-network facility. The payer suggested UW Health bill the patient the full cost, which was tens of thousands of dollars.
These stories may sound like outliers that make the news, but they are among thousands UW Health financial clearance staff deal with annually. (See the sidebar, “More stories of prior authorization challenges from the front lines,” below.)
The staggering price tag
While these stories provide clear evidence of the immediate need for reform of prior authorization processes, the price tag adds even more compelling evidence. UW Health conservatively estimates that the negative financial impact of managing prior authorizations in 2019 for all services (excluding transplant procedures and prior authorizations secured in decentralized clinic locations) was about $18.2 million, roughly $3.6 million of which was lost revenue due to cancellations and rescheduling because of prior authorization delays.
Sixty-five FTEs are needed to handle prior authorizations. Eight additional FTEs are required to notify insurance companies of unplanned, urgent and emergency admissions. Another team in utilization management handles concurrent reviews with insurers, providing insurer updates and handling disputes over inpatient or outpatient status while the patient is admitted. And two denial management staff advocate for patients experiencing denials. Beyond the high cost of staff to manage this administrative burden, there also is the time required by physicians, nurses, schedulers and customer service to coordinate appeals, provide payer-requested clinical information, manage rescheduling and field patient questions.
When calculating these losses, challenges related to prior authorization that are not easily measured, such as the impact of the high turnover rate of financial clearance staff due to job dissatisfaction, must be considered. These roles require someone who not only can manage required administrative tasks, but also is highly adaptable and can tolerate payers’ inefficient processes, such as waiting on hold with insurers for extended periods of time, only to be disconnected. The financial clearance staff must be detail-oriented as they double and triple check prior approvals because of conflicting or outdated payer information. They also must have a high degree of patience and empathy to help patients navigate complex insurance rules that can leave them financially at risk.
7 industry solutions for addressing administrative waste
Solutions for removing waste from the prior authorization processes are within the industry’s grasp. Here are a few industrywide remedies that could be adopted to alleviate the unreasonable burden current prior authorization problems impose on providers:
- Create a standard list of what requires authorization and what does not across all payers and plans to eliminate the guesswork and variation on when authorization is required.
- Require standard electronic submission pathways across all payers to enable automation.
- Shorten the decision-making time from 15 days to seven business days for routine cases. Require that medically urgent determinations be made within 24 hours.
- Require that appropriately documented medically necessary care be covered by the payer, even if prior authorization is not obtained.
- Require transparency through easy-to-access online resources that show when prior authorization is required. (Note: Implementing the standardized list mentioned in #1 could obviate the need for this step.)
- Ensure that changes to policies and rules occur during contract negotiations rather than being rolled out piecemeal during the year.
- Require payers that utilize medical policies to determine medical necessity review the patient against their own policies prior to service if the provider requests that they do so.
The answer may be in the data
In addition to taking these steps, we should probe the underlying sources of administrative waste and inefficiency, including why unnecessarily complex processes like prior authorization have persisted. Data accessibility is one notable source of waste and foundational to a solution. For example, if we could show prior approvals for MRIs have been secured 95% of the time over the past five years, could that persuade payers to eliminate prior authorizations for these procedures? Under such circumstances, payers would be hard-pressed to justify that value is being extracted from MRI prior authorizations. The hitch is that data to drive such discussions and decisions is not readily available, so these inefficiencies persist.
A recent step in the right direction occurred when CMS announced its plans on Jan. 15, 2021, to address the lack of data sharing and access. Select payers, providers and patients will now have electronic access to pending and active prior authorization decisions. This significantly higher level of transparency should help reduce repeated requests for prior authorizations, thereby lowering costs and the heavy administrative burden providers carry.
Some may argue that the timing is not right to tackle more change in the face of the COVID-19 crisis. But we cannot afford not to pursue change. If we can ease administrative and regulatory requirements for healthcare providers, billions of dollars could be directed toward lowering the cost of care, improving care for the medically underserved, increasing the amount of charity care provided to the uninsured, addressing social determinants of health, funding additional research and improving clinical performance through increased training and education.
It is precisely during times of disruption, such as the current pandemic, that we must seize opportunities. We should strive to relinquish bureaucratic red tape and build new processes and systems that make us better stewards of valuable healthcare resources. We can and must do better.
More stories of prior authorization challenges from the front lines
Countless real-life stories highlight the inefficiencies and blatant administrative waste that plagues the prior authorization process – from incorrect information on insurance websites to uninformed payer staff and an ever-changing set of barriers imposed by insurance companies that burden providers with mounting workloads. Here are more stories, in addition to those described in the main article.
Gamesmanship with third- and fourth-party vendors. An insurer with more than 20 million members uses a third-party vendor to manage imaging authorizations and a fourth-party vendor to direct patients to facilities it determined to be lower-cost. This added layer of complexity means that the third-party authorization vendor will not issue an authorization until UW Health staff contacts the fourth-party vendor to gain approval for the patient’s selected location.
As this payer tries to save money, it has shifted the burden of finding a “low-cost” facility to UW Health financial clearance staff. UW Health staff spend, on average, 20 minutes for each patient in conversations with the fourth-party vendor explaining that the patient has already selected their preferred location for services and that UW Health staff will not be calling the patient to ask that they go elsewhere. This policy also puts patients in the middle, sometimes asking them to switch from their preferred location and interrupting continuity of care. Meanwhile, patient care is delayed and hours of administrative time are wasted. Moreover, attempts to find a lower-cost facility often fail, and the original location is used as was planned.
End runs to get approvals from payers. As physicians make choices about what is best for their patients, they deal with barriers over services not being covered or being designated as experimental. Peer-to peer reviews between physicians on the provider side and medical directors on the payer side can successfully overturn denials, but they typically must occur within 48 to 72 hours or the prior authorization denial will be upheld. This limited window is difficult to coordinate with busy providers who may be scheduled in the OR all day and do not have time to wait on hold with a payer for hours.
No-win situations of administrative inefficiency for both providers and patients. The financial clearance staff at UW Health recently managed a patient case that underscores the high stakes communication between providers and insurers. The patient, whose physician had recommended cervical spine fusion, was covered through a large insurer in the Midwest. UW Health attempted to secure prior authorization for the procedure but was informed by the insurer that prior authorization was not required. UW Health then submitted a pre-determination request, which means the insurer reviews the physician’s recommendation for a procedure, treatment or test to ensure that it meets medical necessity requirements. The insurer refused UW Health’s pre-determination request because the payer does not require it and instead suggested that UW Health financial clearance staff read and interpret the payer’s cervical spine fusion medical policy on its website.
The upshot of this approach is that the insurer is placing all responsibility upon the patient’s physician or the financial clearance staff to interpret its often-complex medical policy. This situation runs the risk of the insurer’s denying payment for the service if the physician representing the patient or the financial clearance staff representative does not interpret the policy in the way the insurer intended. In this case, a disputed interpretation of the medical policy could have put the patient at risk for over $20,000 in self-pay costs.





