10 keys to restoring trust in healthcare: a summary
Insights provided during HFMA’s 16th annual Thought Leadership Retreat can help healthcare leaders better manage relationships and perceptions within and across their communities.
Note: This article was adapted from a report on HFMA’s 2023 Fall Thought Leadership Retreat. The full report is available for downloading.
The issue of restoring consumer trust in the U.S. healthcare system encompasses a wide range of concerns. Factors in the perceived loss of trust include anxiety and confusion over costs, entrenched inequity, misinformation about vaccines and other treatments, and data and privacy breaches.
To examine the problem and explore solutions, HFMA’s 2023 Fall Thought Leadership Retreat convened leaders from across the industry Sept. 28-29 in Washington, D.C. The genesis of the event was a report in HFMA’s “Healthcare 2030” series that described the ebb in trust and linked the issue to deteriorating population health outcomes.
“Healthcare is a complicated system, so therefore trust and the opportunity to rebuild or restore [it] — that solution has to be systemic,” C. Ann Jordan, JD, president and CEO of HFMA, said during the retreat. “It’s going to require everyone in this room.”
The retreat represented a step forward, Jordan noted, because the discussions that took place require trust in and of themselves.
As described below, the key takeaways from the retreat can serve as a road map to enhance consumer confidence and clinician faith in the U.S. healthcare system.
1. Defining the issue

One key to solving the apparent trust deficit in healthcare is to precisely understand the goal.
“It’s not so much that our job is to restore trust. Our job is to make ourselves trustworthy,” said Zeev Neuwirth, MD, an author and longtime physician executive, referring to a directive described in the 2000 book The Trusted Advisor.
The issue goes to the heart of the healthcare mission.
“People who don’t trust the healthcare system, they just don’t seek care, and there are going to be higher rates of nonadherence,” said Alexander Ding, MD, MBA, associate vice president for physician strategy and medical affairs with Humana. “People are going to end up being sicker, and it’s going to cost the country a whole lot more in terms of healthcare costs when they have to come in at a much more urgent stage later on.”
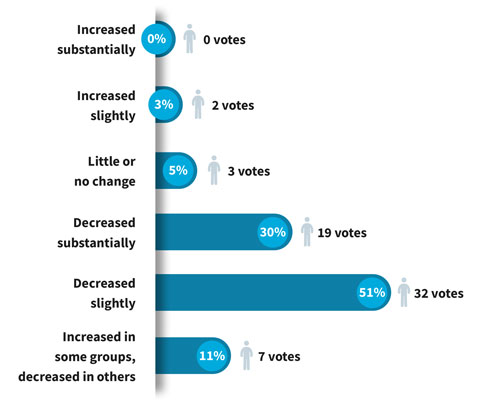
Stakeholder feedback: How has patient trust in healthcare changed since 2020?
2. Measuring trust
Finance leaders and other healthcare stakeholders should strive to rigorously assess the trust their patients and customers have in their organizations.
Neuwirth referred to a formula known as the Trust Equation, which was described in The Trusted Advisor and includes four variables:
Credibility + Reliability + Intimacy
_________________________________
Self-Orientation
Neuwirth singled out the intimacy factor, explaining, “Emotionally, do I connect with you? Do I feel safe? Do I feel I can share with you?”
Self-orientation, the denominator, should be de-emphasized as part of a trusting professional relationship.
“You can have all the confidence and intimacy and reliability you want, but if I believe that you are in this for yourself and you’re not in it for me, that completely demolishes trust,” Neuwirth said.
3. Boosting affordability
A prerequisite for improving trust in the system is to make care more affordable for patients and ensure they have access to needed therapies.
“Under many surveys and assessments, the U.S. [healthcare system] is objectively ranked as the leader in novel scientific innovation, whether it’s through technology companies, new devices, new drugs, etc.,” said Carter Dredge, lead futurist with SSM Health. “But where we fall short as an industry is in affordability and access and equity types of things.”
Dredge described his role as an architect of a model designed to make healthcare more affordable and accessible on a large scale. As seen in Civica Rx, the not-for-profit generic-drug company that launched in 2018 and now counts more than 55 health systems as members, the model can be thought of as a healthcare utility.
The model incites what Dredge called intentional commoditization — in this case, the commoditization of generic drugs that have been on the market for years and are not likely to undergo modification.
The consumer-facing impact is significant, he noted: “We dramatically improve the [likelihood] for patients that when their physician says this is the appropriate therapeutic, they get it.”
4. Increasing value
Even though most patients aren’t aware of the concept of value-based care in technical terms, they appreciate any steps taken by providers to put their whole-person health front and center.
“More than ever, we absolutely need value-based care to build a person-centered health system,” said Purva Rawal, PhD, chief strategy officer with the Center for Medicare and Medicaid Innovation (CMMI). “Our fee-for-service [FFS] payment systems are not designed to meet the needs of patients in a holistic way.”
CMMI works to establish a value-focused infrastructure through mechanisms such as upfront investments in data and other resources for participants, Rawal said. The goal, as set out in a strategic blueprint issued in 2021, is for all FFS Medicare beneficiaries to be in an accountable care relationship by 2030.
“This means that we’re really focused on models that can facilitate longitudinal relationships between providers and patients,” Rawal said. “I think of this as making sure patients have a provider that is quarterbacking their care across settings and across other providers to make sure that their needs are being met — not only their medical needs, but also their health-related social needs.”
5. Healing the clinicians
Healthcare organizations can’t optimally serve consumers without clinicians who are fully engaged. That state is increasingly difficult to achieve amid levels of stress and strain that were a problem before the pandemic and have been exacerbated since.
The term burnout doesn’t capture what’s going on in many cases, Neuwirth said.
“It’s not really burnout,” he said. “It’s actually moral injury.”
Tim Porter-O’Grady, DM, a nurse leader and senior partner for health systems with TPOG Associates, LLC, said engaged nurses have unique opportunities to connect with patients in a way that increases trust in the healthcare system. Thus, for C-suites, a key to improving the system is to involve nurse leadership more directly.
“Do you have people like me sitting at your strategic table so that I can raise the questions that invariably and ultimately will impact your ability to succeed? Because I may not be designing [strategy], but by God, I’ll be implementing, and if I don’t implement it, it’s not going to happen,” Porter-O’Grady said.
6. Improving transparency
The opacity of the healthcare system discourages consumer trust. Stakeholders should be looking at ways to make prices and other key information more transparent and digestible.
Much of the most substantial work is taking place on the health plan side because insurers have the ability to aggregate price information from across a market.
Health plan price transparency files are making progress as accessible tools, said Danielle Lloyd, MPH, senior vice president for private market innovations and quality initiatives with AHIP (formerly America’s Health Insurance Plans). In commercial plans, 50% of enrollees now have the credentials they need to access price-listing apps.
Physicians may be as much in the dark about pricing structures as patients are.
“We don’t understand the financial mechanisms,” said Stephanie Duggan, MD, who at the time was regional president and CEO of Ascension St. Mary’s Hospital in Saginaw, Michigan (in October, Duggan was named chief clinical officer for SSM Health). “In medical school, we’re not taught that.”
She said initiatives to bolster patient trust should be centered on improving those mechanisms.
“We can help on the clinical side, but we have to get the billing piece very transparent, very open and very correct,” Duggan said.
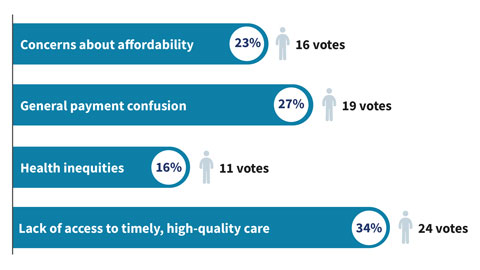
Stakeholder feedback: Which of the following has the most negative impact on patient trust in the U.S. healthcare system?
7. Improving equity
Mistrust in the healthcare system is felt most keenly by demographic groups that historically have lacked opportunities to receive high-value healthcare. The underlying inequity in access and health outcomes must be addressed as a precondition of building trust.

An important step is to further diversify the clinical workforce and other patient-facing staff.
“If you’re a patient of color and you see a physician of color, you assume to some degree that there is some equity in that system,” said Claude Brunson, MD, executive director with the Mississippi State Medical Association.
“We haven’t seen the diversity in healthcare, in people who are taking care of patients or in the system itself,” he added.
Gender equity also remains an issue in some areas. Peter Angood, MD, CEO with the American Association for Physician Leadership, noted that slightly more than half of medical school classes are female, but in a specialty such as surgery, the share is only
about 20%.
AHIP’s Lloyd said her association’s efforts to improve provider directories have included feedback from focus groups indicating that the diversity of a provider’s office staff is important.
8. Going digital
AI will be an increasingly significant presence in healthcare operations in upcoming years, and stakeholders are considering how to ensure the technology increases trust rather than diminishes it.
Digital medicine has the potential to improve healthcare, Neuwirth said. For example, statistics show the average primary care visit lasts 18 minutes, with the physician engaged in data entry or retrieval for more than 16 of those minutes.
“How do you build trust when your eyes are focused on a screen?” Neuwirth said.
Soon, he said, physicians will be able to interact more directly with patients while an automated solution creates better medical notes than any physician can. The technology will even be able to accurately read patients’ emotions.
“That’s the [type of] technology that’s going to rehumanize healthcare,” Neuwirth said.
Beyond technological concerns, Porter-O’Grady said, are the profound differences in leadership structures required for the digital age as opposed to the fading industrial age.
“So much of the leadership that we express is no longer relevant to the world we live in,” he said.
9. Easing systemic friction
An ongoing concern of both patients and clinicians is the type of roadblock to care posed by processes such as prior authorization.

Insurers and regulators understand the reasons for the frustration.
“From our perspective, prior authorization is really key to making sure that our patients are safe, that medicine is practiced [by] adhering to evidence-based care and that we’re keeping coverage affordable,” Lloyd said. “But we fully recognize the process is not so great and that we need a lot of improvement.”
One initiative would promote electronic prior authorization. In a pilot incorporated by an AHIP member in Washington state, 89% of requests were instantaneously approved, and none were instantaneously denied.
“It allows artificial intelligence to be used [so] you can go and pull the documentation out of the electronic health record — without the provider having to do it — and can even use natural language processing,” Lloyd said.
Rawal said CMMI and CMS’s Center for Medicare are looking at ways to test gold carding in Medicare Advantage, giving providers a way to reduce their exposure to time-consuming prior authorization processes.
10. Acting now
Neuwirth paraphrased the architect Buckminster Fuller, who referred to changing systems not by fighting them but by creating a new system that surpasses them. If legacy stakeholders don’t take necessary steps, disruptors that specialize in narrow segments of healthcare could win over growing numbers of consumers.
“I believe that the American public still trusts their providers and their provider systems more than these other entities. That’s a superpower,” Neuwirth said. “And you have your presence in the community. You have those ties, that legacy of relationship, of community service, etc. You have so much power in your people.”
However, he added, “The thing about superpowers is you have to realize you have them and then you have to exercise them.”
That will be especially important for providers as older generations of healthcare consumers give way to millennials and Gen Z, stakeholders said.
“If you don’t exercise your superpowers, you’re going to lose them,” Neuwirth warned.
That’s why the solution road map must yield action.
“It’s time to stop admiring the problem,” said Robyn Begley, DNP, RN, CEO with the American Organization for Nursing Leadership. “Let’s get moving.”
Takeaways from attendees
Small-group discussions involving attendees, whose roles span administrative and clinical leadership positions with providers and health plans, are an annual staple of HFMA’s Thought Leadership Retreat. Here’s a sampling of the insights that came from the discussions on restoring trust in healthcare and from comments offered by attendees during the formal presentations.
Trust and organizational performance. For frontline workers, the visibility, accessibility and believability of executive leadership are critical factors. Leaders need to make themselves consistently available, and if they do, employees will open up to them.
Transparency. Commercial insurers have consumer-friendly apps that can make finding healthcare services more like a retail-shopping experience. Hospitals should be talking to their payer partners about the best way to leverage those tools.
Affordability. Affordability issues and medical debt collection practices are driving deferred care. Patient guidance and navigation at the front end of the financial experience are relatively easy steps that can pay big dividends.
Thank you to our sponsors and partners
HFMA appreciates the generous support provided by the sponsors of the 2023 Fall Thought Leadership Retreat: Humana, Ensemble Health Partners, Equity Quotient, Guidehouse, Turquoise Health and Wells Fargo.
We also extend our appreciation to the American Association for Physician Leadership and the American Organization for Nursing Leadership for their partnership in hosting this event.





