The Quadruple Aim: How robotic-assisted surgery helps organizations provide high-quality care at a lower cost
Enhancing patient satisfaction, reducing healthcare costs, improving healthcare outcomes and enriching the clinician experience: It’s all part of the Quadruple Aim, an expansion of the Institute of Healthcare Improvement’s Triple Aim, which provides a four-prong framework for high-quality patient care and optimal population health.
There are many ways to achieve each individual prong of the Quadruple Aim; however, there are few strategies that address the Quadruple Aim in its entirety. Minimally invasive surgery (MIS) — specifically robotic-assisted surgery (RAS) — is one of them.
This white paper addresses how healthcare organizations can leverage RAS as a financially viable modality to improve physician and patient satisfaction while simultaneously lowering costs, reducing complications and generating new net revenue.
Finding your ‘why’: Getting started with RAS
Finding your ‘why’ is important for any significant capital investment because it helps identify how you’ll measure success. With RAS, every healthcare organization must ask these critical questions:
- Why are we investing in RAS?
- What do we hope to achieve by offering RAS to our providers and patients?
- How will we know once we’ve achieved it?
For example, many healthcare organizations leverage RAS to improve patient outcomes and lower healthcare costs because it has been shown to significantly reduce complication rates and prevent readmissions. How a health system deploys RAS technology is a crucial part of unlocking it’s potential. That was one of the primary reasons why Baton Rouge General, which has been a pioneer in robotics for more than a decade, decided partner with Intuitive Surgical to evaluate and optimize its RAS program.
“We’re chasing zero harm — zero surgical site infections, zero readmissions, zero central line infections,” said Stephen Mumford, chief operating officer at Baton Rouge General. “When you have a high-functioning robotic surgery program, it’s easier to get closer to zero,” said Mumford. “It’s less invasive to the patient, you’ve got smaller incisions, quicker recovery times and patients are back to functioning faster. All of this equates to better outcomes and lower risk of having an adverse event. It made perfect sense for us to get into this space.”
Improving patient outcomes and reducing healthcare costs also paves the way for successful participation in value-based payment arrangements.
“Complications are expensive,” said Mumford. “They cost patients money and anxiety. They also increase expenses for the overall episode of care.” said Mumford added that RAS has helped Baton Rouge General achieve optimal performance in several payer-based accountable care organizations.
“That’s what commercial payers and Medicare care about — the total spend,” said Mumford. “You could have been very cost effective in the operating room, and then the patient gets an infection and must stay an extra week, and you just blew the budget out of the water,” he adds.
Another reason to optimize RAS? Patients want it, says Mumford.
“Over the last five years, patients have become consumers,” said Mumford. “They’re seeking a world-class experience. They’re going to get online and look at who is doing robotic surgery and who is doing it well. They’re becoming data-driven, which I think is great because now they’re making objective decisions on where to go for their care.”
Physicians increasingly want access to well-coordinated RAS programs as well.
“When you look at trying to attract young, talented physicians coming out of residency or fellowship, most of them are training on robotic surgery,” said Mumford. “When you’re trying to recruit the best of the best, if you don’t have the technology, it’s going to be tough.”
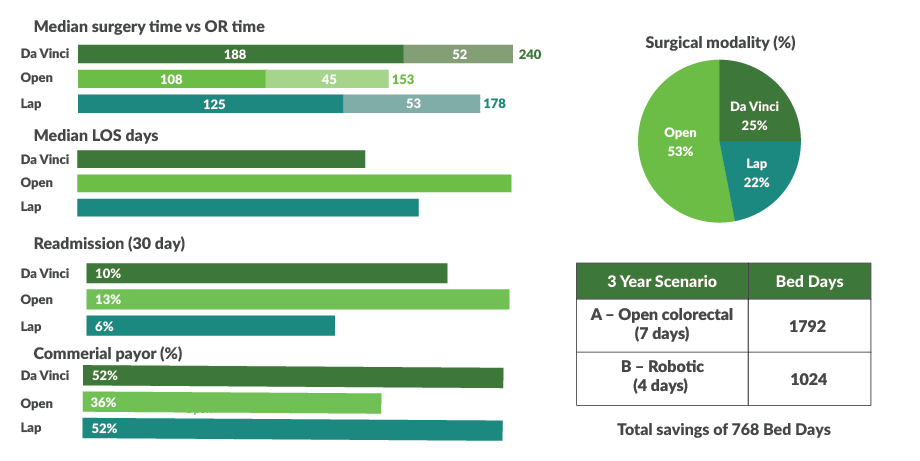
RAS reduced LOS — Consider the full impact
Operational KPIs Colorectal (Benign), 2017-2020
Establishing robotic-assisted surgery as a service line
Organizations that have taken the time to define their ‘why’ have laid the foundation for a successful RAS initiative — one that promotes high-quality patient care at a lower cost and meets each prong of the Quadruple Aim. However, defining your why, purchasing a robot, and establishing clear intentions and goals isn’t enough.
“A lot of organizations buy a robot, and they just let doctors use it as they please,” said Mumford. “As you do that, it will not become the cost-effective revenue generating machine it was designed to be. You must get administrators and clinicians working collaboratively to form a true cohesive group that runs the robotic surgery program.”
How can organizations do this? They must establish robotic-assisted surgery as a service line, emphasizes Mumford. This means dedicating resources to capital investments, staffing, marketing, ongoing training and more.
Here are several ways to establish RAS as a service line within a healthcare organization.
Identify key players, form an RAS steering committee. Typically, key players include a surgeon champion, executive sponsor, operational leader and tactical leader. At Baton Rouge General, the following individuals also serve on the robotics steering committee: Robotics team leader, director of perioperative services, surgeons from all disciplines, chief operating officer, chief nursing officer and operating room manager. A physician and administrator both co-lead the robotics steering committee that reports directly to the Medical Executive Committee.
Answer critical questions. For example, what individuals might the healthcare organization need to hire to create a dedicated team whose goal is to support the RAS program (e.g., specially trained surgeons, nurses, surgical technicians and anesthesiologists)? What specific data will the RAS steering committee review regularly, and why? Will the healthcare organization offer RAS 24/7, 365 days a year or only during normal business hours? Which services lines will leverage RAS, and why?
Meet regularly, share data. This includes organization-specific data that comes directly off the robot console (e.g., the length of time each surgeon stays on the console when performing a procedure, instrument choreography and case spend to improve standardization and reduce variation). “We leverage our partnership with Intuitive to get meaningful data that we can give to our doctors,” said Mumford. “One of the things I like about Intuitive Surgical is that they don’t just sell you a robot. They sell you a partnership and a service. They’re also selling you their commitment to having that robot be a high-functioning machine for your patients. You must choose to take advantage of that.” Baton Rouge General reviews this information that Intuitive Surgical provides in concert with its own internal data (e.g., each surgeon’s average length of stay, cost and infection rates for certain procedures) and then compares trends with national averages. “We can easily see where the variation is — and where there are opportunities for improvement to help us meet the Quadruple Aim,” said Mumford.
Standardize procedures, reduce clinical variation for RAS. Standardizing care for patients who undergo RAS is a top priority at Baton Rouge General, said Mumford. “For example, a surgeon might have found a way to use one less suture to close an incision while achieving the same or better outcomes. By sharing this experience — and standardizing more cost-effective care — that’s when we start to see the benefits of better margins.” Collegiality, transparency, and collaboration make this possible. “We have healthy competition that ultimately benefits patients and drives costs down,” he added. “If you just have the robot in the corner, and physicians come and go and use it as they please, you’re never going to maximize what it can do for you financially,” said Mumford. “There’s no collaboration among the end users who are the physicians. Ten doctors may do the same procedure 10 different ways, and none of them get the insight from the other nine to see if they can improve.”
Have a plan to market the RAS program. Patients will take advantage of RAS only when they know the healthcare organization offers it and that it may be a better alternative to an open or laparoscopic procedure. That’s why marketing the RAS program is important. Mumford says Baton Rouge uses a variety of strategies, including physician podcasts, published patient stories and even onsite hands-on experiences where patients can look at and touch the equipment.
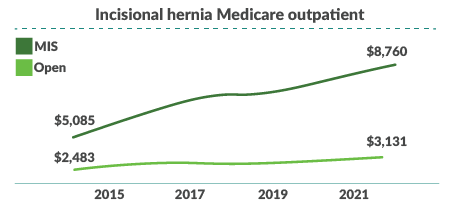
Reimbursement trends favored outpatient MIS
Meeting the Quadruple Aim with RAS
When healthcare organizations leverage RAS as a service line, they’re able to achieve the Quadruple Aim more easily. Consider the goal of providing cost-effective care. Mumford said Baton Rouge General has compared the cost of surgeries performed via open, laparoscopic and robotic-assisted methods.
“When you look at our total spend, most of the time it’s the lowest with robotic. Patients are doing better and have shorter stays,” said Mumford.
Mumford provides the example of a large hernia repair that surgeons can now perform on an outpatient basis using RAS. “Outpatient surgery costs the health plan a quarter of what it would have cost if the patient had to stay in the hospital,” he said. “If we do a same-day hysterectomy or even a hysterectomy with a 23-hour stay as opposed to a four- or five-day stay, imagine how much less that’s going to cost.”
In addition, the health system has used RAS to significantly improve outcomes as well as reduce adverse events, including admissions to the intensive care unit, blood transfusions, conversions to open procedures and surgical site infections.
Improving the patient experience using RAS
Improving the patient experience is one of the goals of the Quadruple Aim, and it’s one that healthcare organizations can easily achieve with RAS, said Mumford.
“No patient wants open surgery anymore, and there’s only a small subset of patients who require it,” he added. “Not only do we want to offer robotic surgery to them; we want to offer it to them at a competitive price, and we want to give them the same outcome or better than they would get with a major vertical incision.”
Enhancing physician retention, satisfaction using RAS
Leveraging RAS as a service line also helps attract and retain top talent, said Mumford.
“When you’re in a competitive labor market, money only goes so far,” he added. “What’s your differentiator from the hospital around the corner or five miles away? It’s the culture and the team. Everyone is committed to high-quality patient care and the best possible outcomes.”
Intuitive Surgical also offers additional advantages that improve the physician experience. More specifically, surgeons can collaborate with others in real time during surgical procedures to ensure patients have the best outcome possible. Surgeons can also record procedures and view them together with patients postoperatively to explain what they did and why. All of this greatly enhances the patient and provider experiences.
Conclusion
Establishing RAS as a service line helps healthcare organizations provide high-quality, cost-effective care that satisfies the Quadruple Aim. However, it takes a team to make this work, and that team must include an innovative technology partner that provides data, ongoing support and best practice strategies to ensure success.
“If your intentions are to buy the robot, leave it there, and hope that it pays for itself in a short period of time, then don’t do it,” said Mumford. “But if you’re interested in robotics as a service line, you’ll see a huge ROI. Go all in as a team of administrators and providers. Make this a high-functioning asset for your patients. Commit to driving high-quality results at a lower cost.”
About Intuitive Surgical
Intuitive®, headquartered in Sunnyvale, Calif., was founded in 1995 to create innovative, robotic-assisted systems that help empower doctors and hospitals to make surgery less invasive than an open approach. Since da Vinci® became one of the first robotic-assisted systems cleared by the FDA for general laparoscopic surgery, it’s taken robotic-assisted surgery from concept to reality. Working with doctors and hospitals, we’re continuing to develop new, minimally invasive surgical platforms and future diagnostic tools to help solve complex healthcare challenges around the world. Innovating for minimally invasive care. It’s the passion that drives us at Intuitive.
This published piece is provided solely for informational purposes. HFMA does not endorse the published material or warrant or guarantee its accuracy. The statements and opinions by participants are those of the participants and not those of HFMA. References to commercial manufacturers, vendors, products, or services that may appear do not constitute endorsements by HFMA.






